On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
Outsourced Insurance Authorization Services

Managing prior authorizations can feel like a never-ending paperwork battle for healthcare providers. Between gathering patient information, verifying insurance eligibility, and following up on approvals, it eats up valuable time that could be spent on patient care. That’s where outsourced insurance authorization services come in—offering a streamlined, cost-effective solution to handle the entire process, ensuring faster approvals, fewer denials, and improved operational efficiency.
In this article, we’ll break down exactly how these services work, the benefits they bring to healthcare providers, and why outsourcing prior authorization is becoming a game-changer in modern healthcare.
What Are Outsourced Insurance Authorization Services?
Outsourced insurance authorization services refer to hiring a specialized third-party company to handle prior authorizations for medical procedures, treatments, and prescriptions. These companies manage everything from collecting patient data to submitting authorization requests and handling follow-ups, ensuring healthcare providers can focus on patient care instead of administrative headaches.
Why Do Healthcare Providers Need Prior Authorization?
Insurance companies require prior authorization to determine if a proposed treatment or procedure is medically necessary and covered under a patient’s policy. However, obtaining these approvals is a time-consuming and often frustrating process that can delay patient care. With insurance guidelines constantly changing, even a minor error can lead to claim denials, revenue loss, and patient dissatisfaction.
By outsourcing this process, healthcare providers can ensure timely approvals, reduce administrative burdens, and improve overall efficiency.
Key Takeaways on Outsourced Insurance Authorization Services
- Reduces Administrative Burden: Outsourcing eliminates the time-consuming process of handling prior authorizations, allowing healthcare staff to focus on patient care
- Speeds Up Approvals: Dedicated outsourcing teams ensure faster authorization processing by submitting accurate requests and proactively following up with insurers.
- Minimizes Claim Denials: Expertise in insurance regulations helps reduce errors and increase approval rates, preventing revenue loss.
- Cuts Costs on Staffing & Training: No need to hire and train in-house staff—outsourcing provides experienced professionals at a lower cost.
- Ensures Compliance with Changing Regulations: Insurance policies frequently change, but outsourcing providers stay updated to maintain compliance.
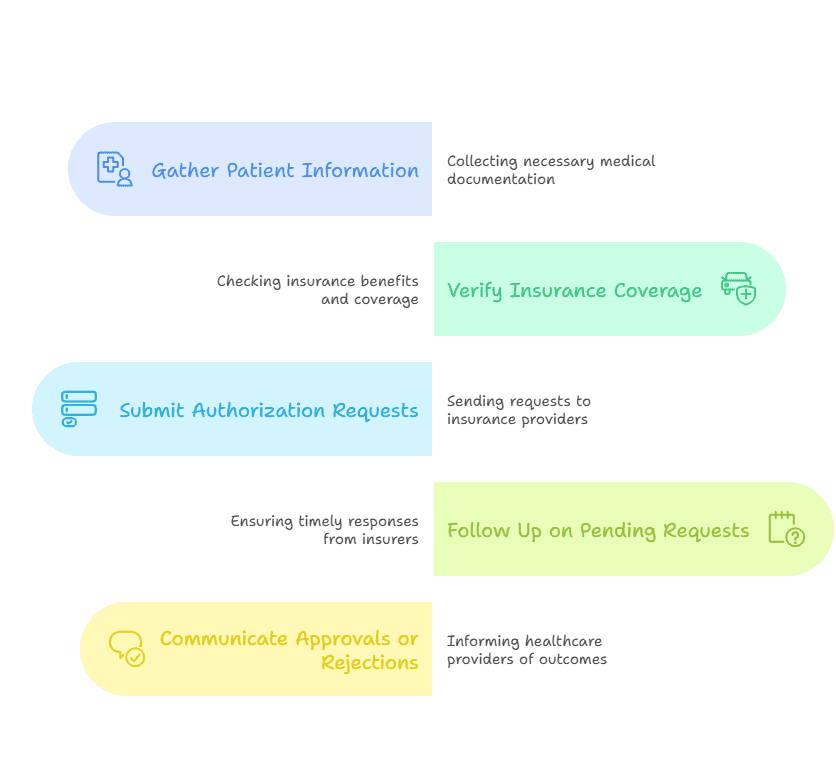
How Do Outsourced Insurance Authorization Services Work?
When a healthcare provider outsources prior authorization, the process typically follows these steps:
1. Patient Data Collection
The provider sends the outsourcing company relevant patient information, including:
- Diagnosis codes (ICD-10)
- Treatment plans (procedures, medications, etc.)
- Insurance details (payer information, policy numbers, etc.)
2. Insurance Eligibility Verification
The outsourcing team checks the patient’s insurance coverage to confirm:
- Policy validity and active coverage
- Authorization requirements for the requested treatment
- Potential restrictions or alternative treatments covered
3. Submission of Prior Authorization Requests
Once eligibility is verified, the outsourcing team submits authorization requests to the insurance company. This includes:
- Filling out required forms based on insurer-specific guidelines
- Submitting supporting medical documents
- Ensuring compliance with payer requirements to avoid denials
4. Continuous Follow-Up & Communication
Insurance approvals don’t always happen instantly. Outsourced teams track pending requests, follow up with insurance companies, and resolve any issues, ensuring faster responses.
- Handling insurance inquiries or additional documentation requests
- Appealing denied requests with necessary corrections
- Providing real-time status updates to healthcare providers
By outsourcing these steps, providers no longer need to worry about keeping up with complex and ever-changing insurance regulations.
Outsourcing Insurance Authorization
1. Reduced Administrative Burden
Prior authorizations require dedicated staff to handle submissions, track approvals, and respond to insurers. Outsourcing eliminates this burden, allowing in-house teams to focus on patient care rather than paperwork.
2. Faster Approvals, Fewer Delays
Outsourced teams specialize in navigating insurance company workflows, reducing approval times and preventing unnecessary treatment delays.
3. Increased Revenue & Fewer Claim Denials
Incorrect or incomplete prior authorization requests often lead to claim denials. Expert outsourcing teams ensure higher approval rates by submitting error-free documentation.
4. Cost Savings on Staffing & Training
Maintaining an in-house team for prior authorization means hiring, training, and retaining staff, which can be expensive. Outsourcing eliminates these costs while providing access to experienced professionals.
5. Compliance with Changing Insurance Regulations
Insurance policies and guidelines change frequently. Outsourcing companies stay updated on these changes, ensuring compliance and reducing the risk of denials due to outdated practices.
6. Improved Patient Satisfaction
When prior authorizations are handled quickly and accurately, patients receive treatments on time, improving their overall experience and trust in the healthcare provider.
| Healthcare Provider Type | Primary Prior Auth Challenge | Outsourcing Benefit | Efficiency Gain |
|---|---|---|---|
| Hospitals & Clinics | High volume processing | 24/7 dedicated teams | 60% faster approvals |
| Specialty Practices | Complex high-cost treatments | Clinical justification experts | 85% approval rate |
| Primary Care Physicians | Referral & diagnostic approvals | Automated eligibility checks | 70% time savings |
| Home Health/Telemedicine | Remote service authorizations | Real-time status tracking | 50% fewer delays |
| Pharmacies | Specialty medication PA | ePA electronic submissions | 90% first-pass success |
Who Can Benefit from Outsourced Insurance Authorization?
Many healthcare providers can benefit from outsourcing, including:
- Hospitals & Clinics – Reduce administrative workload and improve operational efficiency.
- Specialty Practices (Oncology, Cardiology, Orthopedics, etc.) – Handle complex authorizations for high-cost treatments.
- Primary Care Physicians – Ensure smooth approval for referrals and diagnostic tests.
- Home Healthcare & Telemedicine Providers – Streamline authorizations for remote patient care services.
- Pharmacies – Secure approvals for prescription medications requiring prior authorization.
No matter the size or specialty, outsourcing prior authorization ensures smoother operations and better patient outcomes.
Common Challenges in Prior Authorization & How Outsourcing Solves Them
1. Long Wait Times for Approval
🔹 Solution: Outsourcing companies have dedicated teams that expedite the process through continuous follow-ups and insurer-specific expertise.
2. High Denial Rates Due to Documentation Errors
🔹 Solution: Professionals ensure accurate documentation and appeals for denied claims.
3. Lack of In-House Expertise in Insurance Regulations
🔹 Solution: Outsourcing companies stay updated on changing insurance policies to ensure compliance.
4. Rising Administrative Costs
🔹 Solution: Outsourcing is a cost-effective alternative to hiring and training in-house staff.
What Did We Learn?
✅ Outsourced insurance authorization services streamline the prior authorization process, reducing administrative workload and improving efficiency.
✅ They help healthcare providers save time, reduce claim denials, and increase revenue.
✅ Outsourcing ensures compliance with constantly changing insurance regulations, improving approval rates.
✅ Providers across all specialties—from hospitals to pharmacies—can benefit from outsourcing these services.
✅ Faster approvals lead to better patient care and satisfaction.
What People Are Asking ?
1. How long does the prior authorization process take?
Approval times vary depending on the insurance provider and treatment type. However, outsourcing significantly reduces delays through proactive follow-ups.
2. Can outsourcing companies handle appeals for denied claims?
Yes! If a prior authorization request is denied, the outsourcing team can appeal the decision by providing additional documentation or correcting errors.
3. Is outsourcing prior authorization services HIPAA-compliant?
Absolutely. Reputable outsourcing companies follow strict HIPAA guidelines to ensure patient data security and confidentiality.
4. Will outsourcing save my practice money?
Yes! It eliminates the need to hire and train an in-house team, reducing administrative costs while improving efficiency.
5. Do outsourcing companies work with all insurance providers?
Most outsourcing providers are experienced in working with various insurance companies, ensuring seamless processing regardless of the payer.
4.Can small medical practices benefit from outsourcing prior authorization?
Yes! Smaller clinics and solo practitioners often lack the resources for a dedicated prior authorization team. Outsourcing ensures they receive expert support without the overhead costs of hiring additional staff.
5. How do I get started with outsourcing insurance authorization?
It’s simple! Contact Staffingly, Inc., and we’ll assess your needs, integrate with your workflow, and start managing prior authorization requests efficiently—so you can focus on patient care.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services,
please contact Staffingly, Inc. at (800) 489-5877
Email : support@staffingly.com.
About This Blog : This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



