The Financial Impact of Medical Coding
Mistakes in Medical Coding and Billing Impact can be costly. Did you know that nearly 80% of medical bills contain errors? That’s a staggering number. Even small mistakes, like a misplaced modifier or an outdated code, can cause significant financial setbacks for healthcare providers.
For example, let’s say a cardiology practice submits a claim using an incorrect CPT code for a heart procedure. If the code doesn’t match the diagnosis, the insurance company may reject the claim, delaying payment and requiring resubmission. In worst-case scenarios, repeated errors could lead to audits or even compliance penalties. Medical Coding and Billing Impact plays a crucial role in ensuring accurate reimbursements and avoiding financial pitfalls.
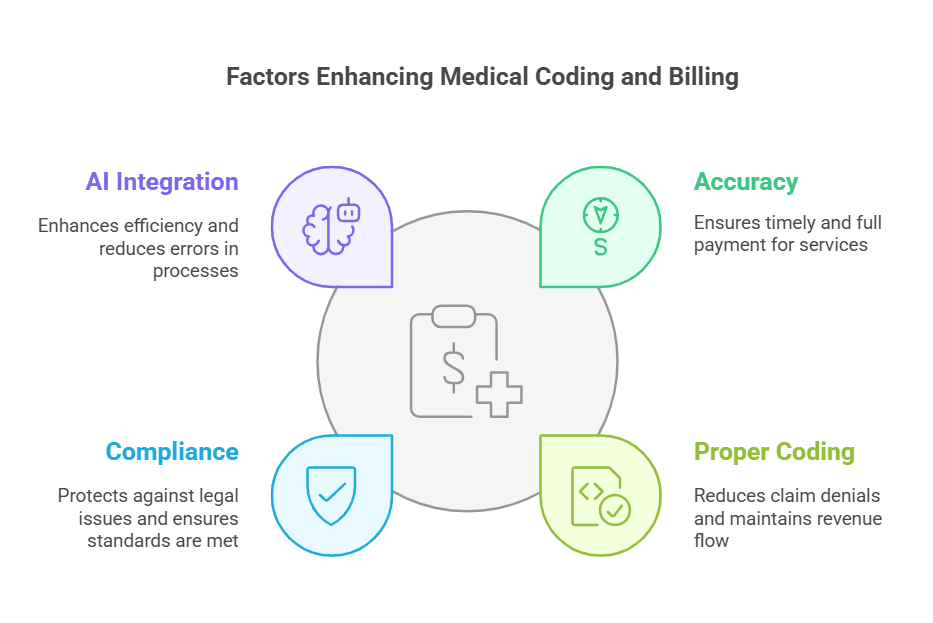
To maintain revenue stability, healthcare providers must prioritize accurate medical coding. Proper training, coding audits, and AI-driven coding solutions can minimize errors, ensuring faster claim approvals and fewer rejections.
| Coding Error Type | Frequency | Financial Impact | AI Prevention |
|---|---|---|---|
| Incorrect CPT Code | 35% of denials [file:2] | $250 avg/claim delay | Automated code suggestion [file:2] |
| Missing Modifier | 25% of errors | 15-30 day payment delay | Real-time claim scrubbing |
| ICD-10 Mismatch | 20% diagnosis errors | Claim rejection + rework | NLP clinical note analysis [file:2] |
| Outdated Codes | 10% compliance risk | Audit exposure + fines | Live code library updates |
| Unbundling Errors | 10% procedural miscoding | Underbilling revenue loss | Predictive denial analytics [file:2] |
AI in Telemedicine Technology: A Game Changer for Medical Coding
Now, let’s sprinkle in some tech talk. Artificial Intelligence (AI) is transforming Medical Coding and Billing Impact, and it’s worth mentioning here. AI is not only improving patient care but also enhancing efficiency and accuracy in medical coding.
Here’s how AI in Telemedicine Technology is revolutionizing the process:
- Automated Coding Assistance: AI-driven tools analyze medical records and suggest the most appropriate codes, reducing human errors.
- Real-Time Claim Scrubbing: AI detects missing or incorrect codes before submission, preventing denials and rework.
- Natural Language Processing (NLP): AI-based medical scribing tools extract relevant details from clinical notes and convert them into billable codes.
- Predictive Analytics: AI can forecast potential claim denials based on past trends, allowing providers to correct errors before submission.
With AI integration, Medical Coding and Billing Impact becomes more streamlined, error-free, and financially efficient. AI can help reduce administrative burdens, speed up claim approvals, and improve overall revenue cycle management.
By implementing AI-driven coding solutions, healthcare providers can increase accuracy, prevent claim denials, and maximize reimbursements—all of which contribute to the financial success of medical practices.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!

 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



