On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
360 Degrees of Revenue cycle management (RCM) process
Author: Sai Teja Inala
Introduction: The healthcare industry in the US is completely different from the healthcare setup in India because people in the US believe in the “Prevention” model rather than the “Cure” model.
- As a result of this strategy, the average lifespan in the US is approximately 75 years, and it is still rising due to improvements in illness management methods.
- A recent survey found that nearly 86% of Americans have health insurance to cover their medical costs.
- The medical insurance industry alone consumes about 18% of the US GDP. The relationships between the three Ps—patient, provider, and payer—are at the center of the healthcare system.
Business Process Outsourcing (BPO): In this case, business is outsourced from developed nations like the US to underdeveloped nations like India. Offshore and inshore outsourcing are two different forms.
- One of the most common management techniques today is offshore outsourcing to India. One should think about outsourcing to other countries, even if this is typically motivated by the desire to save costs.
- The service providers in India will be extremely important in raising quality and productivity in addition to lowering costs.
Role of India in Business Process Outsourcing: India is a key player in BPO because of the following reasons:
- Constant infrastructure improvement
- Liberalized policies
- Qualified personnel
- Political steadfastness
- Financial stability
Healthcare Revenue Cycle Management: HRCM is a thorough procedure that oversees claims processing, payment, and revenue generation by obtaining patient personal and treatment information while maintaining patient confidentiality.
- At present, “value-based care” reimbursement and “quality of life” play a vital role in the healthcare industry.
- It requires technology to monitor the claims process at every stage so the healthcare provider billing may follow the process and address any errors, enabling a consistent flow of income.
- The process includes keeping track of claims in the system, making sure payments are collected, and addressing denied claims, which can cause up to 90 percent of missed revenue opportunities.
The HRCM can be broadly divided into five steps:
- Assessment and Review:
- This is a vital step in enhancing the RCM process.
- When a patient makes an appointment with the physician, the hospital staff will verify the demographics of the patient; check the patient’s active insurance cover; medical & medication history of the patient; and insurance eligibility.
- All these five steps were considered together as a “Pre-registration process.”
- If this process is performed efficiently, the rework throughout the RCM can be drastically reduced, ultimately controlling the denials.
- However, the patient initially needs to pay out of his pocket to receive the services from the hospital or facility. When the claim is paid by the insurance company, the patient will be refunded.
- Claims preparation:
- After the patient’s visit is complete, the healthcare provider needs to submit a claim to the insurance company to receive payment for services.
- To do this, the clinical notes of the physician along with the medical information of the patient need to be converted into electronic health records, this process is termed “medical transcription.”
- This is followed by “Medical Coding,” where the physician or the staff mentions the ICD – 10 or CPT code relevant to the medical condition.
- Finally, the physician will record the information related to the services they provided to the insurance for getting paid and this is known as “Charge capture”.
- Claims Submission:
- Once the claim is prepared, it should be submitted to the insurance company.
- A new claim can be raised in the respective insurance portal, and all the documents related to medical; medication; laboratory; doctor notes should be submitted.
- Apart from this, for the majority of medications and medical procedures, “Prior authorization” is necessary to get the services covered by the insurance.
- To submit a prior authorization request, the physician or the health care team needs to answer all the clinical questions appropriately and should provide the justification to pay for the medication or medical procedure.
- The PA request can be submitted to the insurance company either by raising a claim in the portal or by making a phone call.
- However, platforms like Cover my meds is better suitable to submit a PA request as we can follow up on the request frequently and by using this, we can save time.
- Managing Claims:
- Here, we need to check the status of the claim regularly to know the outcome.
- The insurance personnel will check the claims they receive and make a decision accordingly.
- If the claim meets all the requirements, then it will be “approved or paid.”
- If the insurance company needs any additional information to make a decision about the claim, they will revert back to the facility via fax and will give an outcome upon receiving the same.
- However, if the criteria were not met, then the claim would be “denied or rejected” by the insurance.
- The physician or the healthcare team can check the reason for the denial and can appeal if they think the outcome given by the insurance is not appropriate.
- This is termed “Denial management,” which accounts for 90% of the missed revenue, and should be performed efficiently for the healthy financial management of the hospital or facility.
- Collecting payments:
- Once a claim is paid, the facility or hospital will receive the payment for their services.
- If the patient initially paid out of pocket to get the services, the same amount will be refunded to the patient once the claim is paid.
- Along with this, there are a few aspects related to the claim that the facility personnel needs to know for handling the claims and payments.
- This includes deductibles; co-pay; partially covered; not covered. Based on all these factors, revenue generation will be determined.
- They also assist healthcare professionals to be aware of their revenue cycle status and to receive payment for the services provided.
Challenges for Healthcare Revenue Cycle Management: It can be challenging for organizations to keep their revenue cycle management practices consistent in light of the constantly evolving healthcare laws.
- One of the biggest challenges in revenue cycle management for healthcare businesses is collecting payments from patients at or before the point of service.
- Due to high deductibles and financial difficulties, many patients are unable to pay medical expenses in full upfront.
- Staff members’ coding mistakes result in problems with claim reimbursement.
- The lengthy prior authorization process necessitates that patients delay obtaining or rendering care until the health plan approves.
- The healthcare team will encounter difficulties with things like accurate chart documentation, coding methodologies, and financial policy reminders.
Role of Technology and AI in HRCM: Healthcare revenue cycle management strategies have been streamlined and improved because of systems like Health IT and EHR.
- They support the income by collecting payments, handling claim denials, and tracking claims throughout their lifecycles.
- Artificial intelligence can keep track of massive amounts of data and assist providers in identifying specific indicators, such as why a claim was rejected.
- I. is capable of carrying out tasks more accurately and efficiently with little to no error, such as predicting out-of-pocket expenses or claim coding.
- I. can assist physicians in suggesting ICD-10 codes, keeping track of medical billing procedures, and even scheduling patient appointments.
Influence of Denials on Health Care Revenue Cycle Management:
- As per the article “The Change Healthcare 2020 Revenue Cycle Denials Index”, there is an increase in the denials rate by 23 % since 2016.
- The COVID – 19 pandemic has had a great influence on denials. Especially there is a 14 % denials rate in the Pacific and Northeast regions of the U.S.A.
- 86 % of the denials are preventable and if addressed properly, can be a major source of income.
- Lack of proper resources, inadequate training for staff, and shortage of qualified personnel are the major reasons for the increase in denials.
- Implementing Artificial Intelligence methodologies will help in controlling the denials. Especially the A.I. will provide insights related to medical coding.
- Percentage of Denials: Year-Wise:
| Year | 2016 | 2019 (2nd Half) | 2020 ( 1 Q) | 2020 ( 2 Q) | 2020 ( 3 Q) |
| Percentage (%) | 9 | 9.5 | 10 | 10.8 | 11.1 |

B. Factors Contributing to Denials:
| Factors: | Eligibility | Invalid Claim
Data |
Authorization | Service Not covered | Medical Documentation | Medical Necessity | Untimely Filing | Medical Coding | Provider Eligibility | Avoidable Care | Unknown |
| Percentage: | 26.6 | 17.2 | 11.6 | 10.6 | 9.2 | 6.6 | 5.4 | 4.8 | 0.9 | 0.7 | 6.4 |

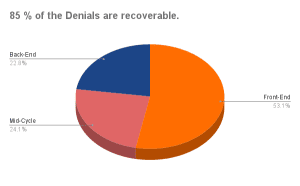
C. Denials Based on Phases of RCM:
| Phase | Front-End | Mid-Cycle | Back-End |
| Percentage | 49.7 | 22.6 | 21.3 |
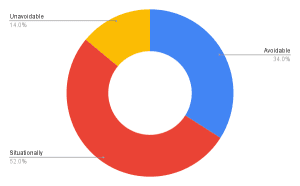
D. Denials can be prevented:
| Avoidable | Situationally Avoidable | Unavoidable |
| 34% | 52% | 14% |
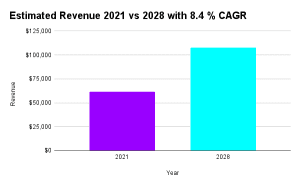
E. HRCM Market Growth Forecast:
| Year | Revenue | Estimated CAGR |
| 2021 | $ 61440 | 8.4 % |
| 2028 | $ 107880 |
Importance of Medical Coding in preventing the Denials:
- Mentioning the accurate ICD – 10 or CPT code can reduce the denials to a greater extent.
- For example, while working on analgesics, we need to mention the diagnosis code based on the underlying medical conditions.
a. If the patient is on analgesic and if he/ she was diagnosed with a malignant neoplasm or cancer chemotherapy, then “G89.3” should be mentioned as a diagnosis.
b. If the patient was diagnosed with trauma, fracture, or accident, and is on analgesics for a longer duration, then “G89.21” should be mentioned.
c. Similarly, if the pain is chronic and because of a procedure or surgery, then “G89.28” should be mentioned.
d. If the pain is chronic, but the cause is not particular then G89.4 should be used.
e. The chances of denial will be very high if the code is inaccurate. “ R52 or Pain, unspecified” is a classic example of the same.
3. For anemia, the diagnosis code should be based on underlying medical conditions.
a. If the patient was diagnosed with renal failure, then “D63.1” should be mentioned as a diagnosis.
b. If the patient was diagnosed with neoplastic disease then “D63.0” should be mentioned.
c. If the patient is on cancer chemotherapy, then “D64.81” should be mentioned.
d. If the diagnosis is any other chronic condition like congestive heart failure, then “D63.8” can be mentioned.
e. Whereas for iron deficiency anemia, the diagnosis code should be decided based on the underlying cause for anemia. For e.g., “D50.0” should be used for “Iron deficiency anemia due to blood loss”.
f. If “D64.9” is mentioned as a diagnosis for anemia, the chances of denials will be very high since the code is not specific.
References:
- www.relias.com/blog/the-role-of-healthcare-revenue-cycle-management
- https://revcycleintelligence.com/
- https://www.hfma.org
- https://www.devry.edu/blog/healthcare-revenue-cycle-management.html
- https://pubmed.ncbi.nlm.nih.gov
- Change-Healthcare-2020-Denials-Index-Report%20December%202020.pdf
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



