On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
Will AI Really Replace Medical Billing and Coding in Healthcare?
A healthcare billing specialist recently posted:
“Do you guys see medical billing and coding being replaced by AI, or is it unlikely? Have you used AI at your work yet?”
That single question sparked a heated debate among coders, RCM experts, and healthcare administrators.
Some said their hospitals already use AI for claim scrubbing and coding. Others shared horror stories of “hundreds of denials” from basic errors.
One coder summed up the sentiment:
“AI saves time, but we spend twice that fixing what it breaks.”
Healthcare professionals across the discussion agreed on one thing — AI may change billing and coding, but it can’t replace human expertise.
Legacy Systems Still Holding Healthcare Back
Many professionals said healthcare’s outdated infrastructure is what’s blocking effective automation.
One physician wrote:
“This is still a field that uses fax machines and printed Excel sheets. The tech isn’t ready for AI — the foundation’s broken.”
Another billing manager added:
“If anything, offshoring is a bigger issue than AI. At least humans can learn from their mistakes.”
The reality? Hospitals and clinics still depend on manual data entry, fragmented workflows, and unstructured documentation.
AI thrives on clean, consistent data. When fed inconsistent or incomplete information, AI amplifies human errors — it doesn’t fix them.
Healthcare automation only works when organizations first standardize their workflows. Until then, coders and billers remain the last line of defense against revenue loss.
Real-World AI Coding Errors and Denials
Multiple professionals shared how AI-created coding errors caused financial chaos.
“Our hospital used AI for office visits and simple procedures. I found hundreds of denials for a basic Z-code error. The AI coded a history code as primary — and nothing else.”
Another coder reported:
“We use AI a lot at my site. Then we use people to manually fix all the AI-created issues.”
Instead of saving time, poorly managed AI often pushes errors downstream, where deadlines have already passed.
When claims go unpaid, providers lose revenue permanently due to missed filing windows.
“You can’t file clean claims with dirty data,” said one denial manager. “AI or not, accuracy still matters.”
Vendor Hype vs. Clinical Reality
Billing teams expressed frustration over how aggressively vendors are pushing AI as a full replacement for coders.
“AI can’t read between the lines,” one coding supervisor said. “It doesn’t understand clinical context.”
Others pointed out that professional associations are marketing automation more than it’s ready for:
“AI is being pushed hard by AHIMA. It’s not there yet. It should handle repetitive E/M checks, not complex claims.”
Many worry that leadership decisions are based on cost-saving hype, not operational readiness.
“Even if the software fails, they won’t admit it,” said one billing manager. “They’ll just say the humans were inefficient.”
The sentiment across forums is clear — AI can help, but only under human oversight.
Human Oversight Keeps the Revenue Cycle Safe
Despite automation pressures, healthcare professionals overwhelmingly agree: AI cannot replace coders and billers.
“AI for appeals is awesome. It saves time. But you still need a human to double-check everything.”
“Think of AI as a tool, not a threat,” another coder advised. “It can reduce the number of billers, but it won’t eliminate them.”
The reality is a hybrid model — where AI automates repetitive work and humans handle judgment, exceptions, and payer communication.
AI handles:
Claim scrubbing
-
Denial triage
-
Time-based E/M documentation checks
Human specialists handle:
-
Coding accuracy
-
Compliance reviews
-
Complex payer interpretation
-
Appeals and corrections
As one expert summarized:
“If humans are needed at the start, they’ll be needed at the end too.”
AI + Human Model in Action
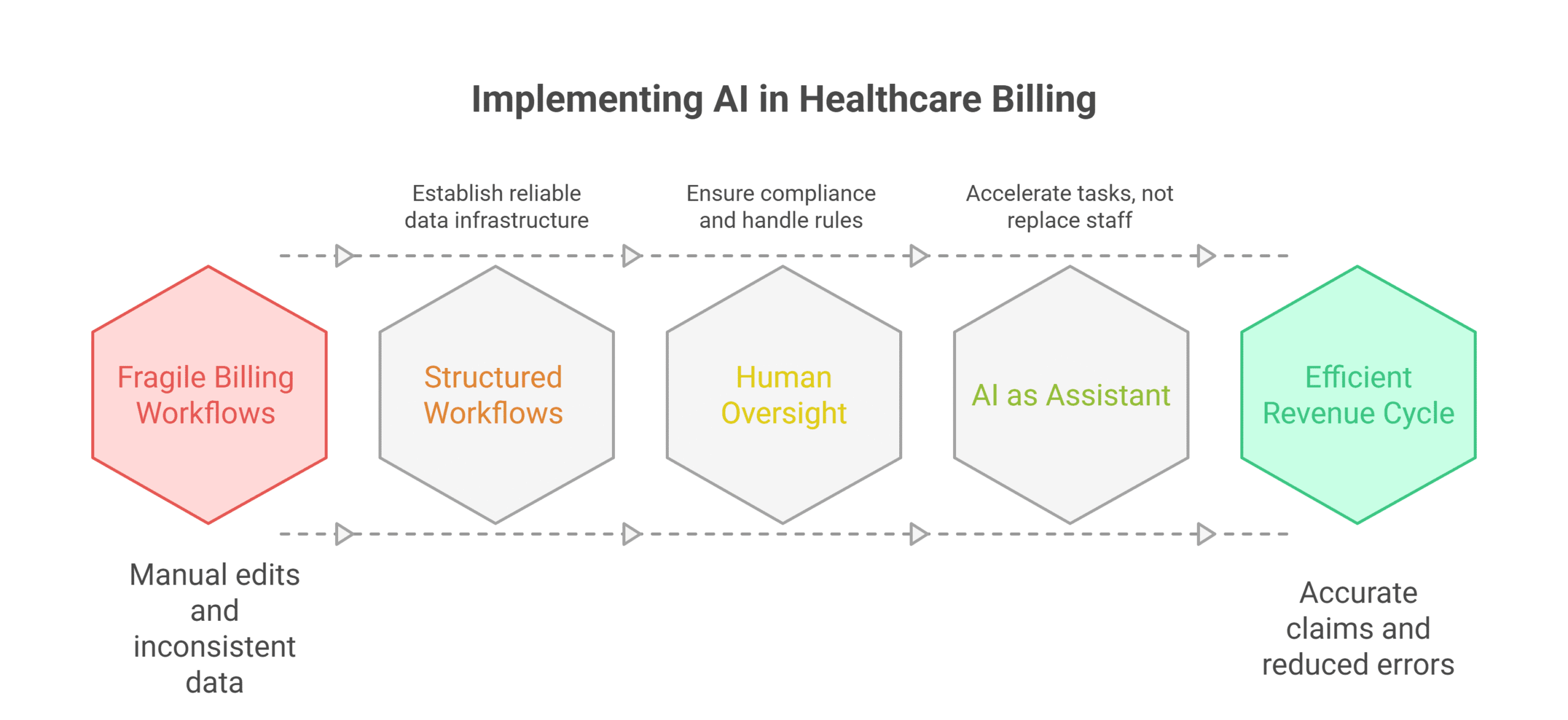
Smart healthcare organizations are embracing AI-assisted Revenue Cycle Management (RCM) rather than full automation.
AI speeds up workflows, identifies patterns, and flags inconsistencies.
Human oversight ensures compliance, accuracy, and patient-level understanding.
This model has proven results:
-
Faster denial resolution
-
Reduced billing turnaround times
-
Stronger payer compliance
-
Fewer revenue leaks
It’s not about choosing between AI and humans — it’s about combining them for precision and protection.
How Staffingly Delivers Hybrid Billing Excellence ?
Staffingly helps healthcare organizations transition into a smarter RCM workflow — where AI efficiency meets human judgment.
✅ Medical Billing & Coding Specialists – Handle AI-generated errors, correct coding, and ensure compliance
✅ Revenue Cycle Management Experts – Prevent denials, optimize claims, and manage appeals
✅ AR Follow-Up & Collections – Recover missed payments and maintain payer relationships
Staffingly specialists are based in India, Pakistan, and the Philippines, bringing medical, pharmacy, and nursing degrees to every engagement.
Each team member is trained on U.S. healthcare billing, CPT/ICD coding, and major EMR systems.
Compliance, Cost, and Global Operations
All Staffingly operations are certified under:
-
HIPAA – Patient privacy and data security
-
SOC 2 – System and organizational control standards
-
ISO 27001 – Global information security
Cost comparison:
-
U.S.-based coder: $4,500–$6,000/month
-
Staffingly virtual specialist: $9.50/hour (~$2,000/month full-time)
That’s a savings of up to 70% per role, while maintaining compliance and quality.
“Our denial rate dropped by 40% after shifting to hybrid coding oversight,” one client reported. “AI + humans finally works.”
Stop Losing Revenue to AI Coding Errors
AI Alone Can’t Protect Your Bottom Line — Skilled Coders Can.
Don’t wait for denials to pile up. Pair AI automation with trained human oversight and get accurate claims the first time.
15-Day Medical Billing and Coding Trial – Risk-Free
✓ Virtual Coding & Billing Specialists – Correct AI errors and ensure clean claims
✓ Revenue Cycle Management Experts – Manage appeals and protect reimbursements
✓ AR Follow-Up & Collections – Recover delayed payments efficiently
HIPAA, SOC 2, ISO 27001 compliant.
Healthcare-trained specialists from India, Pakistan, and the Philippines.
Starting at $9.50/hour — under $2,000 monthly vs $6,000 local hires.
What Did We Learn?
-
Legacy billing systems make AI harder to deploy effectively.
-
AI-generated coding errors cause denials and lost revenue.
-
Vendor hype often overstates AI’s real capabilities.
-
Human oversight ensures compliance and protects reimbursement.
-
Hybrid AI + Human workflows improve accuracy and efficiency.
-
Outsourcing RCM saves up to 70% without losing quality.
What People Are Asking?
Q1. Can AI replace medical coders?
No. AI can assist, but complex cases still need human expertise.
Q2. Will staff roles shrink in hospitals?
Yes, for routine tasks — but auditing, appeals, and oversight roles are expanding.
Q3. Where should hospitals start with AI?
Start small: claim scrubbing, denial triage, and appeals automation.
Q4. Can outsourcing improve accuracy?
Yes. Hybrid virtual teams ensure both speed and precision.
Q5. How much can clinics save with virtual RCM teams?
Up to 70% cost savings, plus faster reimbursements.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services
Please contact Staffingly, Inc. at (800) 489 5877
Email: support@staffingly.com
About This Blog: This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



