On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
Why Insurance Eligibility Verification Is the First Step to Healthy Revenue ?

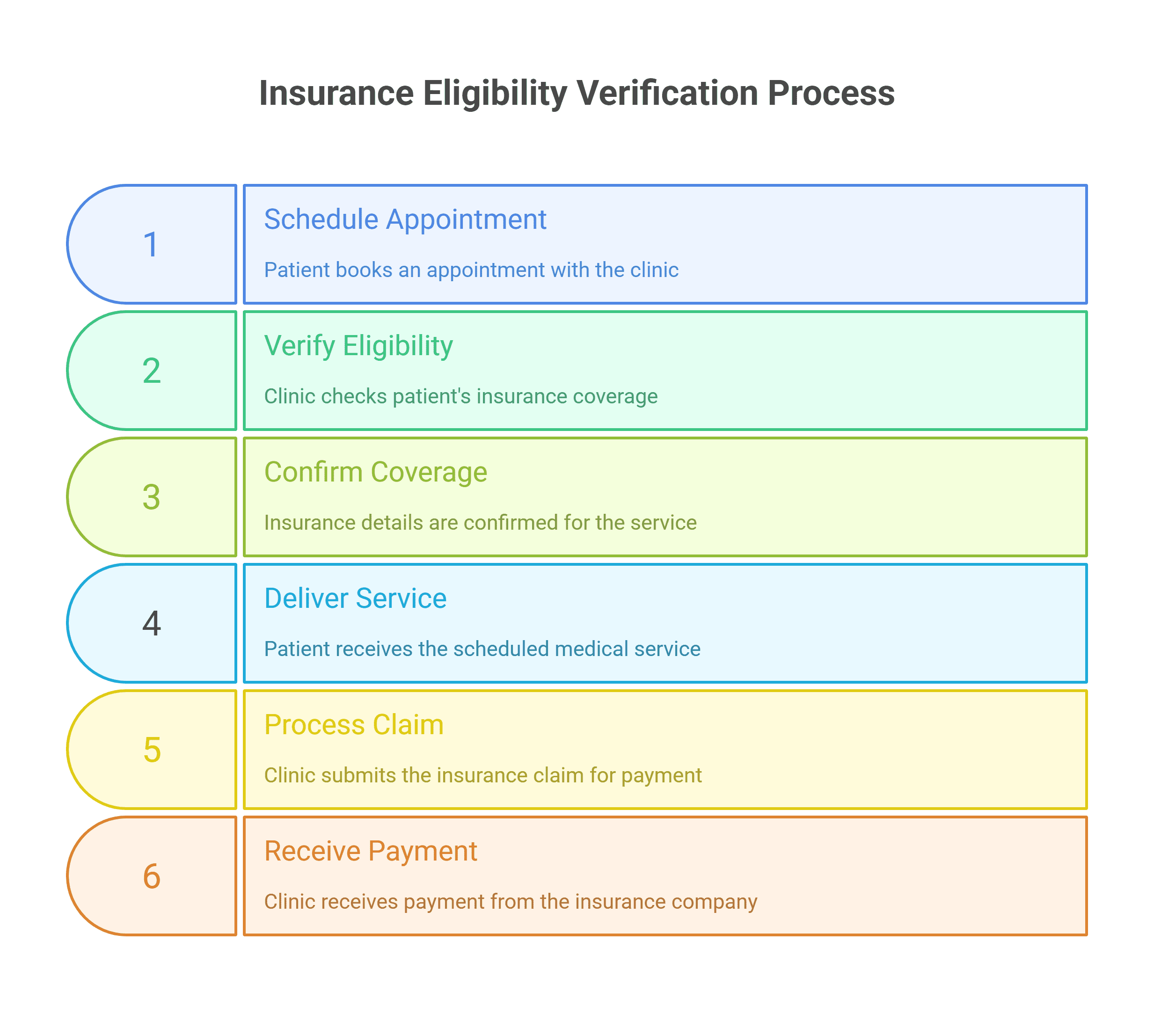
Ask any clinic why revenue slips through the cracks, and they’ll usually blame denied claims or coding errors. But the truth is, most of those problems start much earlier at the point of insurance eligibility verification.
On paper, it’s simple: confirm coverage before a visit. In reality, skipped or rushed eligibility checks cause denials, delayed payments, angry patients, and a financial mess that could have been avoided.
💬 “We had thousands in claims denied just because coverage wasn’t verified upfront.”
Eligibility verification may not be glamorous, but it’s the first and most critical step to protecting both cash flow and patient trust.
Why Eligibility Verification Matters ?
Insurance verification ensures that:
-
Patients are covered for the services they’re scheduled for.
-
Clinics know copays, deductibles, and out-of-pocket costs before care is delivered.
-
Claims won’t bounce back because of inactive coverage or wrong plan details.
Without it, clinics face:
-
Surprise denials that take months to appeal.
-
Staff wasting hours fixing errors after the fact.
-
Patients blindsided with unexpected bills.
💬 “Nothing destroys patient trust faster than handing them a bill for something they thought was covered.”
The Cost of Getting It Wrong
Skipping eligibility checks doesn’t just create headaches it drains revenue:
-
Denied Claims: Insurers reject services not covered, leaving providers unpaid.
-
Delayed Payments: Claims corrections slow down reimbursement cycles.
-
Lost Productivity: Staff spend time reworking claims instead of moving forward.
-
Patient Attrition: Frustrated patients may switch providers.
💬 “By the time we caught the error, the patient had already left the practice.”
Why Clinics Struggle With Verification ?
If eligibility checks are so important, why do clinics miss them?
-
Time Pressure: Staff juggling phones, check-ins, and insurance don’t always have bandwidth.
-
Complex Payer Rules: Every insurer has unique systems and requirements.
-
Manual Processes: Faxing, portal logins, and phone calls create endless delays.
-
Limited Training: Front desk staff may not know what to look for in coverage details.
💬 “I spent 40 minutes on hold just to confirm a copay amount. It’s impossible to keep up.”
Smarter Solutions That Actually Work
The good news: eligibility verification doesn’t have to be a bottleneck. Clinics that succeed focus on automation, specialization, and outsourcing.
-
Automated Eligibility Tools
-
Systems integrate with EMRs to auto-check coverage in real-time.
-
Copays, deductibles, and limits appear instantly during scheduling.
💬 “We stopped chasing denials once eligibility was confirmed at booking.”
-
-
Dedicated Verification Teams
-
Specialists handle insurance checks exclusively.
-
They know payer quirks, codes, and escalation steps.
💬 “Having a remote team verify coverage freed our front desk to focus on patients.”
-
-
Outsourcing for Scale
-
HIPAA-compliant outsourcing teams verify eligibility across all payers.
-
Clinics cut costs while ensuring every patient is cleared before their appointment.
💬 “Outsourcing eligibility was cheaper than hiring another staff member and far more reliable.”
-
A Smarter Way Forward
Eligibility verification may be the least visible step in healthcare admin but it’s the one that makes or breaks revenue. By automating checks, assigning specialists, or outsourcing the process entirely, clinics protect their bottom line and strengthen patient trust from the very first appointment.
That’s where we come in. At Staffingly, we provide dedicated eligibility verification specialists who ensure every patient encounter starts on solid ground so providers can focus on care, not coverage chaos.
What Did We Learn?
Insurance eligibility verification isn’t just paperwork it’s the foundation of revenue integrity.
-
Missed verification leads directly to denials, delays, and lost patients.
-
Staff shouldn’t shoulder the burden alone dedicated teams and automation provide relief.
-
Outsourcing ensures consistency, compliance, and scalability.
-
The sooner eligibility is verified, the healthier the revenue cycle becomes.
What People Are Asking
Q: Why is insurance eligibility verification so critical?
A: Because it prevents denied claims, improves cash flow, and ensures patients aren’t surprised by unexpected bills.
Q: How does eligibility impact patient satisfaction?
A: Patients feel secure knowing costs upfront. Transparency builds trust and reduces billing disputes.
Q: Can automation handle eligibility verification?
A: Yes. Tools can auto-check payer databases, confirm coverage, and flag issues before the visit.
Q: Does outsourcing eligibility save money?
A: Absolutely. Outsourced teams handle checks faster and more accurately, often reducing admin costs by up to 70%.
Q: Is it secure to outsource insurance verification?
A: Yes with HIPAA, SOC 2, and ISO 27001 compliance, plus signed BAAs, data security is guaranteed.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services
Please contact Staffingly, Inc. at (800) 489-5877
Email: support@staffingly.com
About This Blog: This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



