On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
Why Hospitals Are Turning to Outsourcing and What It Means for Patients

Healthcare professionals are raising concerns about outsourcing easy cases to the private sector and the potential creation of a two-tier health system. The discussion highlights critical workforce challenges that public health systems face when simpler cases are redirected to private providers, leaving public facilities overwhelmed with complex cases and inadequate staffing.
The concern centers on resource allocation and whether public healthcare systems can maintain quality care when private providers cherry-pick straightforward cases while public hospitals handle the most challenging and resource-intensive patients.
The Workforce Strain Behind Two-Tier Concerns
When private providers handle routine cases, public health systems face a workforce paradox. They’re left managing complex, time-intensive cases with the same staffing levels that previously handled a mix of simple and complicated patients.
Public healthcare facilities report that administrative burden increases even as patient volume shifts. Staff still process referrals, coordinate care transitions, and manage documentation for patients moving between public and private providers. The administrative overhead doesn’t decrease proportionally with patient volume.
Healthcare professionals note that routing decisions, insurance coordination, and care continuity all require additional staff time when cases are split between public and private systems. The result is often increased workload for existing staff rather than the anticipated relief.
Administrative Burden of Split Healthcare Systems
Managing patient flow between public and private providers creates significant administrative complexity. Healthcare facilities must coordinate:
Patient eligibility verification for private provider access becomes a time-consuming process. Staff members spend hours determining which patients qualify for private outsourcing based on case complexity, insurance status, and provider availability.
Care coordination between public and private facilities requires dedicated personnel to manage handoffs, ensure documentation transfers properly, and maintain continuity. Each patient moving between systems requires verification calls, records requests, and follow-up coordination.
Billing and payment reconciliation becomes more complex when cases split between public and private providers. Staff must track which services were provided where, ensure proper coding for split care, and manage payment flows between different systems.
The Case Complexity Challenge
Healthcare professionals point out that categorizing cases as “easy” or “complex” isn’t straightforward. What appears simple during initial assessment can become complicated quickly. When private providers have first access to seemingly straightforward cases, public systems end up with patients whose conditions evolved or were misclassified.
Public healthcare facilities report that they become the safety net for cases that private providers decline or discharge when complications arise. This creates an uneven distribution where public systems handle a disproportionate share of genuinely difficult cases without corresponding resource increases.
The clinical judgment required to properly route patients adds another layer of administrative work. Healthcare professionals must evaluate each case carefully to determine appropriate placement, a process that takes time and expertise.
Virtual Administrative Support: A Solution Healthcare Systems Are Adopting
Healthcare systems facing administrative strain from complex care coordination are discovering that virtual medical assistants provide cost-effective support for the increased workload.
Virtual administrative specialists handle the time-consuming coordination tasks that multiply when healthcare delivery splits between public and private providers. These professionals manage eligibility verification, care coordination calls, documentation transfers, and follow-up scheduling without requiring additional on-site space or infrastructure.
HIPAA, SOC 2, and ISO 27001 compliance provides enterprise-level security for patient data, ensuring virtual teams meet the same privacy standards as on-site staff. Healthcare facilities maintain full data protection while extending their administrative capacity.
Cost structures make virtual support particularly attractive for public healthcare systems with budget constraints. Virtual specialists starting at $9.50/hour, under $2,000 monthly for full-time support, compare favorably to local administrative staff costing $4,500 base salary plus payroll costs and benefits totaling up to $6,000 monthly.
Insurance Verification and Eligibility Coordination
When healthcare delivery splits between public and private providers, insurance verification becomes exponentially more complex. Each patient referral to a private provider requires verification of eligibility, benefits coverage, and authorization requirements.
Virtual insurance verification specialists systematically check patient eligibility before appointments, confirm coverage details, and identify any authorization requirements. This proactive verification prevents scheduling patients for private provider appointments they aren’t eligible for, reducing wasted coordination effort.
Benefits verification for split care arrangements requires checking coverage across multiple service types and providers. Virtual specialists trained in insurance coordination handle these complex verifications efficiently, understanding the nuances of public vs. private provider coverage.
Healthcare professionals with medical backgrounds understand clinical workflows and terminology, enabling them to ask the right questions during insurance verification calls. U.S. licensed Pharmacists and overseas MHAs provide specialized expertise in navigating complex coverage scenarios.
Medical Scribing and Documentation Support
Documentation requirements increase when patients receive care across multiple settings. Virtual medical scribes help healthcare professionals maintain thorough records without adding to their administrative burden.
Chart preparation before appointments ensures providers have complete patient histories including services received from other facilities. Virtual scribes compile records from multiple sources, creating comprehensive summaries that support quality clinical decision-making.
Real-time documentation support during patient encounters allows providers to focus on patient care while scribes handle EHR data entry. This maintains productivity even when dealing with complex cases that require extensive documentation.
After-visit documentation completion ensures records accurately reflect care provided and support proper coding and billing. Virtual scribes familiar with medical terminology complete documentation thoroughly, reducing claim denials from insufficient documentation.
| Operational Area | In-House Public System | With Outsourcing | Impact |
|---|---|---|---|
| Administrative Cost per FTE | $55,000-$65,000/year | $18,000-$24,000/year | 60-65% cost reduction |
| Claims Processing Time | 30-45 days | 12-18 days | 40-55% faster turnaround |
| Eligibility Verification Accuracy | 85-88% | 96-98% | Up to 13% improvement |
| Denial Rate for Complex Cases | 18-22% | 10-13% | 35-45% reduction |
| AR Days Outstanding | 55-65 days | 30-38 days | Up to 25 days improvement |
The Revenue Impact of Two-Tier Systems
Public healthcare facilities often face revenue pressures when straightforward, well-reimbursed cases shift to private providers while they retain complex, resource-intensive cases with challenging reimbursement profiles.
Virtual revenue cycle management specialists help public facilities maximize reimbursement for the complex cases they manage. These professionals handle claims submission, denial management, and appeals with expertise that improves collection rates.
Medical billing and coding accuracy becomes critical when managing complex cases that involve multiple procedures and diagnoses. Virtual billing specialists with healthcare educational backgrounds including Medical Doctors, Nurses, and PharmDs ensure clinical understanding combined with operational expertise in coding.
AR follow-up and collections require systematic attention that many public facilities struggle to provide with limited staff. Virtual collections specialists systematically work accounts receivable, following up on unpaid claims and resolving payment issues that might otherwise be written off.
Prior authorization specialists navigate the complex approval requirements for treatments and procedures common in the complicated cases public facilities manage. They handle forms, payer portals, follow-ups, and appeals, reducing treatment delays and improving revenue capture.
Staffing Solutions That Scale With Demand
Healthcare facilities dealing with variable administrative demand from split care arrangements benefit from virtual staffing models that flex with workload.
Virtual medical assistants provide coverage for patient calls, scheduling coordination, and follow-up management without the fixed costs of full-time on-site staff. Healthcare facilities can scale support up during high-demand periods and adjust as needs change.
Telemedicine support helps public facilities extend access when in-person appointments are limited. Virtual assistants handle patient onboarding, platform management, and technical support, enabling healthcare providers to see more patients remotely.
Medical triage specialists assess patient needs and route them appropriately, ensuring patients access the right level of care whether through public facilities or private providers. This improves efficiency and patient satisfaction.
The contractor-based model provides flexibility that traditional employment doesn’t offer. Healthcare facilities access specialized expertise without long-term employment commitments, adjusting team size as operational needs evolve.
Stop Administrative Overload From Split Healthcare Systems
Public healthcare facilities managing increased administrative complexity from two-tier healthcare arrangements need support that scales with demand without straining already-tight budgets. Virtual administrative specialists provide the coordination capacity healthcare systems need to manage patient flow across multiple providers effectively.
30-Day Healthcare Administration Trial
✓ Virtual Medical Assistants – Handle patient coordination, scheduling, and follow-up calls across multiple care settings
✓ Insurance Verification Specialists – Verify eligibility and benefits before private provider referrals, reducing coordination waste
✓ Medical Scribing Support – Maintain complete documentation across split care arrangements without adding provider burden
Flexible staffing that adjusts to administrative demand. Clinical understanding from healthcare-educated professionals. Systematic coordination that ensures continuity.
HIPAA-compliant. Healthcare-specialized starting at $9.50 to $12.00/hour. Under $2,000 monthly vs up to $6,000 local staff costs.
What Did We Learn?
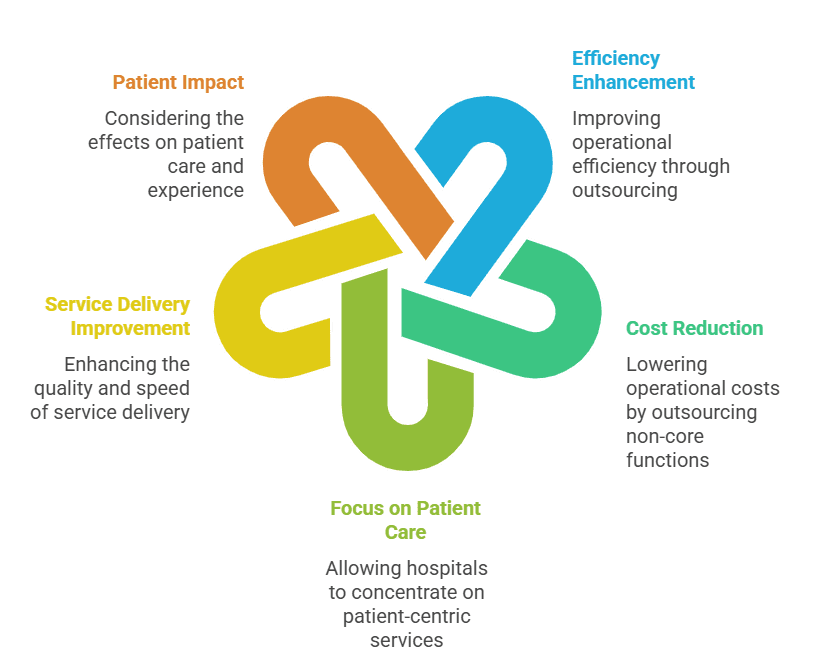
From exploring why hospitals are turning to outsourcing, we learned that healthcare outsourcing has become a strategic response to growing financial pressures, staffing shortages, and administrative burdens within hospitals.
Hospitals are increasingly relying on third-party vendors to manage both clinical services (like imaging, lab testing, and equipment maintenance) and non-clinical services (like billing, credentialing, and IT). This shift helps healthcare organizations cut costs, access specialized expertise, and focus more on patient care.
However, the discussion also highlights important cautions — while outsourcing can improve efficiency and technology adoption, it may also create disparities in care, reduce staff control, and shift focus from patients to profit if not managed carefully.
In essence, outsourcing is a double-edged sword:
-
It can enhance hospital operations when implemented strategically and transparently.
-
But it can also risk patient equality and quality of care if cost-cutting overshadows compassion and accountability.
What people are Asking?
1. What is healthcare outsourcing?
It’s when hospitals hire outside companies to handle services like billing, lab work, IT, or equipment maintenance.
2. Why do hospitals outsource?
To reduce costs, save time, access skilled experts, and focus more on patient care.
3. What are the benefits?
Lower expenses, faster service, advanced technology, and better efficiency.
4. What are the risks?
Possible quality issues, data privacy concerns, job losses, and unequal access to care.
5. How does it affect patients?
Patients may get quicker results but could face inconsistent quality or reduced personal attention.
6. Does outsourcing really save money?
Usually yes, in the short term — but long-term results depend on vendor quality and hospital oversight.
7. What’s the future of healthcare outsourcing?
It’s growing fast, especially in billing, telehealth, and AI-driven services, but must balance cost with patient care.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services,
please contact Staffingly, Inc. at (800) 489-5877
Email : support@staffingly.com.
About This Blog : This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



