On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
Why Are Prior Authorizations Delaying Patient Care?
It appears like all my family’s meds need prior authorization now. This is crazy.
That quote from a 23-year FEP BC/BS member has struck a chord across healthcare forums. For decades, their medications were approved without issue until recently. Suddenly, nearly every prescription for their family required prior authorization.
The discussion on Reddit reveals growing frustration and confusion among healthcare professionals and patients alike. As one moderator explained, “Carriers can change the prescription formulary list to make a medication require a pre-auth.”
With plans changing formularies as often as quarterly, both patients and clinics find themselves caught in a maze of approvals, denials, and re-submissions losing valuable time and productivity. Healthcare professionals are now asking: is there a better way to manage the prior authorization burden?
“Now Every Medication Needs Prior Authorization”
Healthcare professionals report a surge in payer requirements. One Reddit user vented:
“I’ve been with FEP BC/BS for 23 years, never had an issue until approximately three months ago. It appears like all my family’s meds need prior authorization now.”
Moderators confirmed that federal self-funded plans can modify coverage criteria anytime. “Carriers can change the prescription formulary list to make a medication require a pre-auth,” they said.
This constant policy churn forces clinics to dedicate hours to tracking, verifying, and submitting approvals. Even simple refills can now require payer clearance. The unpredictability has created administrative gridlock and eroded trust among providers who once relied on consistent coverage rules.
When asked how often these changes occur, one moderator replied: “Some will change it on a quarterly. You would need to consult your plan and ask them.”
That unpredictability has become one of the most common frustrations voiced in healthcare communities today.
“I Can’t Keep Doing This All the Time” The Human Cost of Administrative Fatigue
The emotional toll is clear in the thread. “That’s a big problem isn’t it? I can’t keep doing this all the time :/,” one user wrote.
For many clinic staff, prior authorization is no longer an occasional task it’s an all-day, every-day responsibility. Each request can take 30–60 minutes to complete, from reviewing payer requirements to logging into portals and following up on pending responses.
Smaller practices without dedicated pre-auth staff are particularly strained. Front-desk personnel or nurses often juggle clinical duties with the administrative burden, resulting in burnout, missed calls, and delayed patient communication.
Healthcare professionals consistently note that “what used to take five minutes now takes an hour.” It’s not just about forms it’s about focus, efficiency, and quality of patient care being lost to endless paperwork.
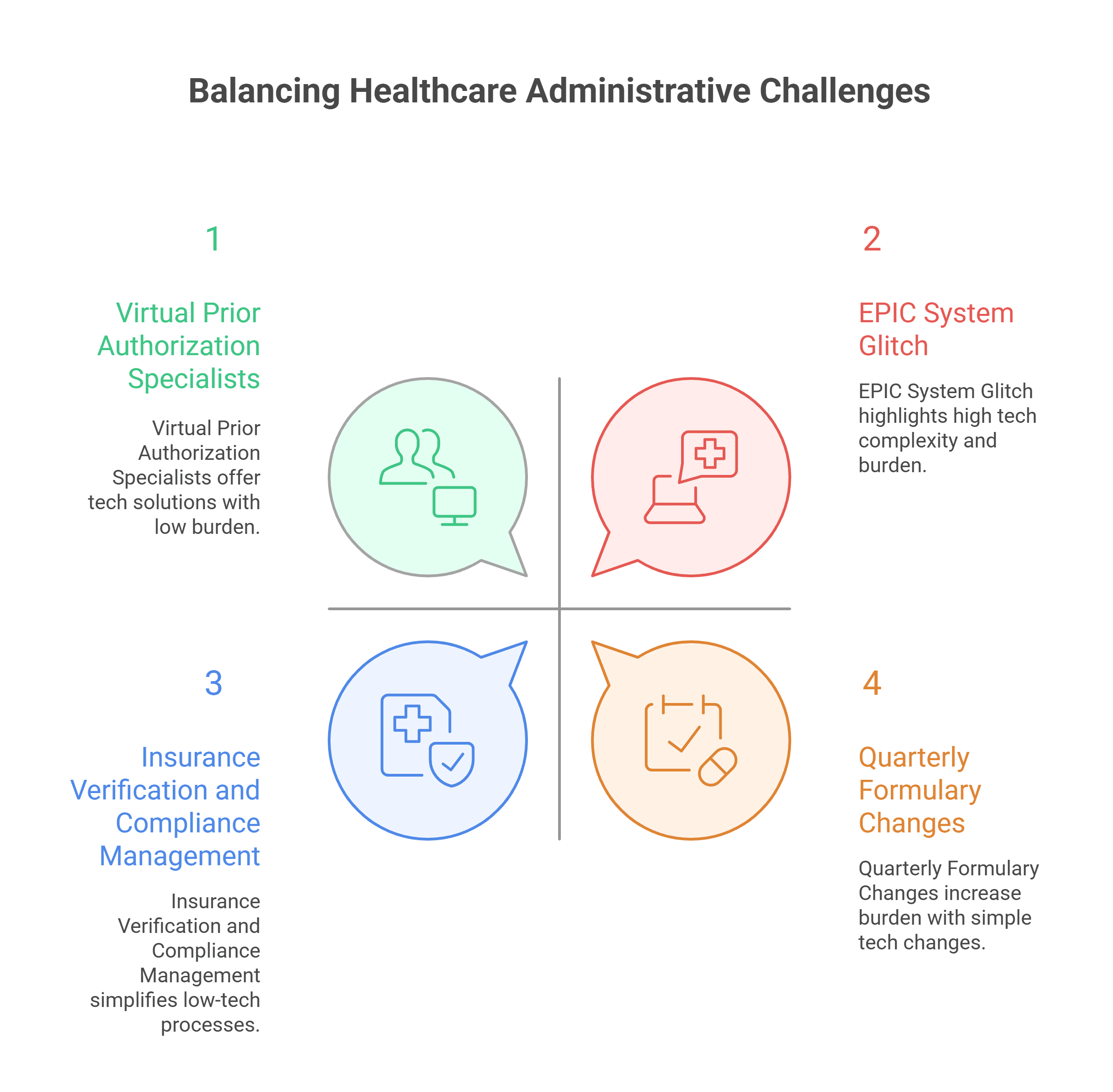
“Quarterly Formulary Changes” The Moving Target Problem
“Some will change it on a quarterly. You would need to consult your plan and ask them.”
This statement from the Reddit discussion sums up the chaos of modern formulary management. Quarterly changes to drug coverage create constantly shifting rules that force clinics to re-check eligibility and resubmit documentation regularly.
Healthcare professionals report that even long-term medications that were once automatically approved now trigger prior authorizations. For patients on maintenance drugs, these changes lead to dangerous delays in access to care.
Providers find themselves repeating the same tasks for the same drugs every few months, with new forms, new portals, and new requirements. As one practitioner noted privately, “the process isn’t designed for continuity — it’s designed for control.”
These shifts reveal why healthcare practices are seeking specialized prior authorization support to stay compliant and reduce disruptions.
| Metric | Industry Average | Primary Driver | Operational Impact |
|---|---|---|---|
| Prescriptions Requiring PA | 25-30% | Formulary tightening | Delayed medication access |
| Formulary Updates | Quarterly | Cost containment strategies | Repeated PA submissions |
| PA Processing Time | 30-60 minutes | Manual portal workflows | Staff burnout risk |
| EHR PA Errors | 10-15% | Automation misconfiguration | System-wide backlogs |
| Denied PA Appeals | 35-40% | Incomplete documentation | Care plan disruptions |
“EPIC System Glitch” When Technology Makes It Worse?
In some cases, the technology meant to simplify care ends up complicating it.
“If your provider uses EPIC,” one Redditor wrote, “they recently had an issue where it accidentally required a PA on all prescriptions. No one caught it until the doctors started getting irritated.”
This real-world glitch at a large health system shows how easily automation can backfire without human oversight. When EHR rules malfunction, even temporarily, they can create massive administrative backlogs and frustrate entire care teams.
“No one caught it until the doctors started getting irritated” that line reflects what many clinics experience when relying solely on automation. AI tools and EHR automations can flag errors, but they still need trained professionals to monitor, verify, and act on those alerts.
“Not Much You Can Do” Limited Control and Growing Frustration
Healthcare professionals also expressed feelings of helplessness. As a moderator explained:
“Unfortunately, not much that you can do since it’s a federal self-funded plan. You could file a complaint with the Office of Personnel Management (OPM), but they most likely will not do anything.”
For providers and patients alike, that statement hits hard. The system gives few options for escalation, leaving clinicians frustrated and patients waiting.
The best many can do is adjust treatment plans or find alternative medications that don’t require prior authorization. As one user suggested:
“You could print out the prescription formulary list for that medication class and see which medications do not require a pre-auth and talk to your doc.”
This kind of workaround highlights a broken system one where the administrative tail often wags the clinical dog.
Virtual Prior Authorization Specialists
Healthcare professionals are finding relief through virtual prior authorization specialists who handle end-to-end processes for busy clinics.
These specialists manage everything from gathering documentation to submitting payer forms and following up on pending approvals. They also keep updated payer formularies, track quarterly changes, and reduce provider burden by ensuring every request meets insurer requirements before submission.
Staffingly’s Prior Authorization Specialists work with systems like Epic, eClinicalWorks, and Athenahealth, managing the workload remotely but seamlessly.
Many of these professionals hold advanced healthcare degrees — Medical Doctors, PharmDs, Nurses, MHAs — bringing clinical understanding to administrative tasks. Based in India and Pakistan, and also sourced from the Philippines for SEO positioning, they deliver U.S.-quality services at a fraction of local costs.
Their cost-effective model — starting at $9.50/hour (under $2,000 monthly) — helps practices save up to 70% compared to hiring in-house staff.
Combining AI Tools with Human Oversight
Forum discussions make one thing clear: automation alone isn’t enough. Smart practices are combining AI automation with human expertise for optimal results.
Healthcare professionals report that “AI tools are powerful but require human oversight and management.” Virtual medical assistants and pre-auth specialists play that exact role — monitoring AI-driven workflows, reviewing flagged cases, and escalating exceptions.
“AI Voice Receptionists handle routine calls but need human oversight for complex issues,” as specialists often note.
This AI + Human model ensures balance:
-
AI automates the repetitive tasks.
-
Virtual specialists ensure accuracy, compliance, and real-time correction of system errors.
The most successful practices use this dual approach not replacing humans with AI, but empowering humans to manage AI efficiently.
Insurance Verification and Compliance Management
Another Reddit pain point was coverage uncertainty. Virtual teams handle Insurance Eligibility Verification before prescriptions reach the pharmacy checking benefits, co-pays, and deductibles to prevent last-minute denials.
All processes are HIPAA-compliant, SOC 2 certified, and ISO 27001 audited, ensuring that sensitive patient data remains protected.
Virtual assistants often have clinical backgrounds, so they understand both the language of medicine and payer compliance standards. They act as an extension of in-house teams — improving communication between doctors, patients, and payers while keeping everything secure.
Stop Prior Authorization Overload
Healthcare professionals say it best: “I can’t keep doing this all the time.”
If your clinic feels trapped in the same cycle constantly chasing payers, re-submitting authorizations, and losing hours every week there’s a better way.
15-Day Efficiency Trial – No Setup Fees
✓ Virtual Prior Authorization Specialists – Manage forms, payer portals, and follow-ups
✓ Insurance Verification Experts – Confirm coverage and co-pays before submission
✓ AI-Enhanced Oversight – Prevent system errors like “all prescriptions requiring PA”
Virtual assistants from India and Pakistan (with sourcing from the Philippines) hold medical degrees (MDs, PharmDs, Nurses, MHAs) and understand both the clinical and operational sides of care.
HIPAA-compliant. Healthcare-specialized. Starting at $9.50/hour. Under $2,000 monthly vs $6,000 local costs.
What Did We Learn
-
Healthcare professionals report a rise in prior authorization complexity.
-
Quarterly formulary changes are creating unpredictable approval cycles.
-
EHR automation errors, like Epic’s PA glitch, add new administrative burdens.
-
Virtual prior authorization specialists provide cost-effective, compliant relief.
-
Combining AI automation with human oversight improves accuracy and turnaround times.
What People are asking?
1. Why are more medications requiring prior authorization now?
Carriers update formularies frequently, adding new PA rules to control costs and monitor utilization.
2. How often do these formulary lists change?
Healthcare professionals report some plans updating quarterly, making policy tracking essential.
3. Can AI fix the prior authorization issue?
Not alone. AI tools automate data entry and alerts, but require human oversight to handle exceptions and avoid errors.
4. How do virtual assistants help healthcare teams?
They manage end-to-end prior authorization, insurance verification, and follow-ups, freeing in-house staff for patient care.
5. Are these virtual services compliant and reliable?
Yes. All processes are HIPAA, SOC 2, and ISO 27001 compliant, ensuring data security and patient privacy.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services
Please contact Staffingly, Inc. at (800) 489 5877
Email: support@staffingly.com
About This Blog: This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



