On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
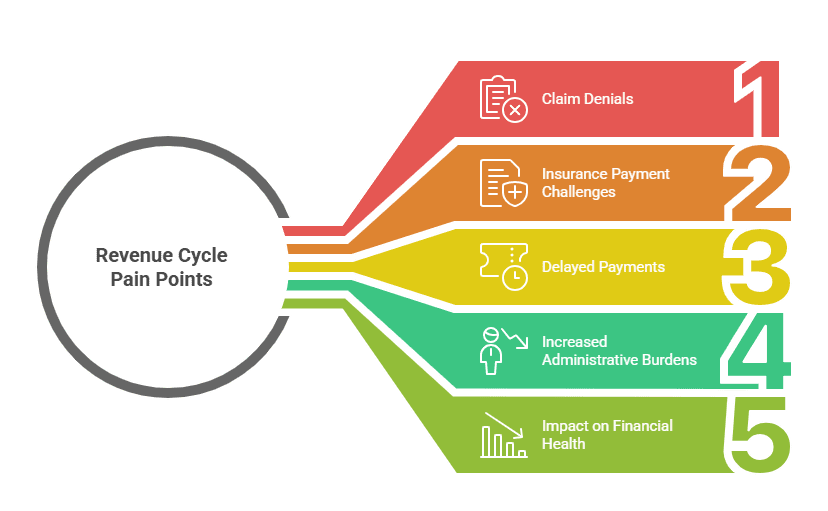
Revenue Cycle Pain Points: Claim Denials and Insurance Payment Challenges

Healthcare professionals active in online forums are sounding the alarm about a troubling revenue problem. Medical practices are quietly losing 10–15% of their revenue simply because claims aren’t being managed aggressively enough. In one recent forum discussion, a medical billing specialist posed a critical question to the community: “What’s your biggest roadblock in RCM right now? Claim denials piling up? Prior authorization delays? Staff overwhelmed with AR follow-ups?” The flood of responses revealed just how deeply revenue cycle management problems are affecting small to medium practices, with systematic failures preventing legitimate claims from ever getting paid.
The Payer Negotiation Trap Small Practices Can’t Escape
Healthcare professionals consistently point to payer negotiations as their most insurmountable barrier. One physician captured the frustration perfectly: “For me, by far its payer negotiations. It ranges from very difficult to impossible to get better pay from insurance companies when you’re small.” Another practitioner was even more blunt: “Payer negotiations which is almost non existent for small to medium practices.”
The reality is stark—small practices often can’t negotiate with insurance companies at all. They’re forced to accept whatever rates payers offer, creating a revenue shortfall before a single claim is even filed.
Forum discussions also expose a dangerous myth circulating in medical billing circles. When one billing specialist confidently stated that commercial payers generally cover 100% of Medicare-approved amounts, an experienced physician consultant quickly corrected the misconception: “idk who told you that generally commercial payers cover 100% Medicare but you are very wrong about that unless you are in a very rural market or you only do specialist RCM.” The consultant added a sobering reality: “Most people I consult with are making well under Medicare from commercial payers.”
This reimbursement gap doesn’t exist in isolation. Combined with high denial rates and slow collections, it creates a compounding financial crisis that small practices struggle to survive.
| Denial Cause | % of Denials | Revenue Impact | Prevention Focus |
|---|---|---|---|
| Eligibility Errors | 25–30% | Delayed or lost payments | Real-time eligibility checks |
| Missing Prior Authorization | 20–25% | High-value claim denials | PA tracking & follow-ups |
| Coding & Modifier Errors | 15–20% | Downcoding & rework costs | Coder audits & training |
| Credentialing Issues | 10–15% | Rejected claims | Upfront credential accuracy |
| Missed AR Follow-Ups | 10–15% | Permanent revenue loss | Dedicated denial workflows |
When Claims Slip Through the Cracks: The AR Follow-Up Crisis
Experienced healthcare professionals report that accounts receivable management quickly becomes overwhelming. One practitioner explained the daily reality: “Honestly, the AR follow-ups and denials are usually the biggest headache. It’s easy for claims to slip through the cracks when staff is already juggling so much.”
The core issue isn’t knowledge—it’s capacity. Practices understand what needs to be done, but lack the staff bandwidth to do it systematically.
Healthcare professionals emphasize the cascading nature of the problem: “Insurance denials are one of those things that can quietly kill momentum in a practice. Every payer has different requirements, timelines, and appeal processes, and if you’re not tracking closely it adds up to lost revenue fast.” Forum members report seeing denied claims that never get appealed within payer deadlines, transforming temporary denials into permanent revenue loss.
One experienced practitioner shared the solution: “What helps is treating denials like their own workflow: flag them quickly, categorize the reason, assign a responsible person, and measure how long they take to resolve.” The challenge? This structured approach requires dedicated staff time that overwhelmed practices simply don’t have. As one honest practitioner admitted: “It’s not glamorous work, but having that structure can turn denials from a constant headache into a manageable process.”
The Upstream Problem: Credentialing Errors That Create Downstream Denials
Healthcare professionals with deep RCM expertise identify a critical upstream problem that most practices overlook. One stated bluntly: “Credentialing has to be done correctly to ensure claims are not rejected later due to modifiers or any other stupid issues.”
The connection between proper credentialing and reduced denials is repeatedly confirmed in forum discussions. A billing specialist explained the logic: “If a company has a strong credentialing and charge posting team, there are fewer issues with denials. Most issues have been addressed during the credentialing process, and knowledge is shared with charge entry.” Another professional confirmed: “If the credentialing and charge entry team is working correctly, the number of denials and rejections will decrease.”
The key insight from healthcare professionals is prevention. Proper setup eliminates problems before they require expensive rework. Most preventable denials can be avoided entirely with systematic credentialing and charge entry processes—but small practices rarely have specialized staff dedicated to this oversight.
The Vicious Cycle: When Overwhelmed Staff Can’t Break Free
Healthcare professionals recognize a brutal truth: billing problems stem directly from staffing limitations. When practices lose “10–15% of revenue just because claims aren’t managed aggressively,” the root cause is almost always billing staff overwhelmed with competing priorities.
The math creates an impossible situation. Local billing staff typically cost practices $4,500 in base salary plus payroll taxes and benefits—reaching up to $6,000 monthly per position. For small practices already managing razor-thin margins and poor payer rates, adding sufficient billing staff becomes financially impossible.
Forum discussions reveal the vicious cycle this creates: insufficient billing staff leads to claim delays and denials, which reduces revenue, which makes it harder to hire additional staff to fix the problem. Practices find themselves trapped, watching revenue leak away while unable to afford the resources needed to stop it.
Virtual RCM Specialists: Breaking the Cycle With Systematic Expertise
Smart healthcare practices are discovering a way out of the staffing trap. Virtual revenue cycle management specialists provide the systematic approach that overwhelmed internal staff can’t maintain—at a fraction of traditional staffing costs.
These specialists bring impressive credentials. Many hold advanced healthcare degrees including Medical Doctors, Nurses, and PharmDs from India and Pakistan, with companies also sourcing talent from the Philippines. Several possess U.S. pharmacy licenses and MHA degrees, combining clinical understanding with billing expertise. This healthcare knowledge proves critical—they understand the clinical context behind claims, dramatically improving accuracy.
What Virtual RCM Specialists Actually Do?
Systematic Denial Workflows: Virtual teams implement the exact structured approach forum discussions recommend: flagging denials immediately, categorizing reasons systematically, assigning clear responsibility, and measuring resolution time. This systematic process directly addresses the “claims slipping through the cracks” problem that practices report.
Dedicated AR Follow-Up Capacity: With virtual specialists handling AR management, practices gain dedicated capacity for the “not glamorous work” of systematic follow-ups. This prevents the permanent revenue loss from claims that never get pursued.
Credentialing and Charge Entry Expertise: Virtual teams with healthcare backgrounds ensure proper credentialing and charge entry from the start, eliminating the “stupid issues” that cause unnecessary rejections.
Cost Structure That Actually Works: Virtual RCM specialists typically cost starting at $9.50/hour—under $2,000 monthly for full-time specialist coverage, compared to up to $6,000 monthly for local staff. The $4,000+ monthly savings per position makes it financially feasible to have sufficient billing capacity for the first time.
Enterprise-Level Security: HIPAA, SOC 2, and ISO 27001 compliance provides the security standards healthcare practices require, with fully managed compliance oversight.
Why Systematic Denial Management Can’t Happen Without Dedicated Capacity
Healthcare professionals emphasize a critical distinction: denial management isn’t complex—it’s time-intensive. The workflow that prevents revenue loss requires consistent, focused attention: “treating denials like their own workflow: flag them quickly, categorize the reason, assign a responsible person, and measure how long they take to resolve.”
Experienced practitioners report what happens when internal staff are “juggling so much”: the systematic approach breaks down at every step. Claims get flagged but not categorized. Denials get categorized but not assigned. Assigned denials don’t get pursued within payer timelines.
Virtual RCM specialists provide dedicated capacity specifically for denial management workflows. The systematic approach actually gets implemented consistently rather than becoming another process that internal staff don’t have time to maintain.
Stop Losing 10-15% of Revenue to Claim Denials
Healthcare professionals consistently report that practices are losing 10–15% of revenue because claims aren’t managed aggressively. The problem isn’t that internal staff don’t understand denial management—they simply don’t have the capacity to implement systematic workflows while “juggling so much.”
30-Day Revenue Recovery Guarantee
✓ AR Follow-Up & Denial Management – Systematic workflows that prevent claims from “slipping through the cracks”
✓ Credentialing & Charge Entry Oversight – Prevent rejections before they happen with proper setup
✓ Prior Authorization Specialists – Handle payer portals, forms, and follow-ups to prevent authorization delays
Get dedicated RCM capacity without overwhelming costs. Healthcare-specialized virtual teams with Medical Doctors, Nurses, and PharmDs handle the systematic work that recovers lost revenue.
HIPAA-compliant. Healthcare-specialized starting at $9.50 to $12.00/hour. Under $2,000 monthly vs up to $6,000 local staff costs.
What Did We Learn?
-
Claim denials and delayed insurance payments remain the biggest pain points in revenue cycle management (RCM).
-
The most common causes include eligibility errors, missing prior authorizations, coding mistakes, and payer down coding.
-
These issues directly impact practice cash flow, staff productivity, and overall revenue.
-
Proactive strategies like denial prevention, real-time eligibility checks, staff training, and automated RCM tools can significantly reduce denials.
-
Successful practices focus on front-end accuracy and back-end follow-ups to ensure smoother claim payments.
What people are Asking?
Q1. What are the most common reasons for claim denials in healthcare?
The most common reasons include eligibility errors, missing prior authorizations, incorrect coding, lack of medical necessity documentation, and duplicate claims.
Q2. How do insurance payment delays affect healthcare providers?
Payment delays create cash flow problems, increase administrative workload, and reduce revenue efficiency, making it harder for providers to maintain financial stability.
Q3. What strategies help reduce claim denials?
Providers can minimize denials by verifying patient eligibility upfront, ensuring accurate coding, using denial management tools, training staff, and conducting regular audits.
Q4. What is denial management in revenue cycle management (RCM)?
Denial management is the process of identifying, analyzing, and resolving denied claims to recover lost revenue and prevent future denials.
Q5. How can technology improve insurance payment challenges?
AI-driven RCM tools, automated eligibility checks, and claim scrubbing software can streamline processes, reduce errors, and speed up reimbursements.
Q6. Why do payers downcode claims?
Insurance companies may down code claims when documentation doesn’t fully support the level of service billed, resulting in lower reimbursements.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services
Please contact Staffingly, Inc. at (800) 489 5877
Email: support@staffingly.com
About This Blog: This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



