On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesREVENUE CYCLE MANAGEMENT(RCM) PROCESS

Author: SHALU KUMARI
ABSTRACT
Revenue is defined as “income, especially when of an organization and of a substantial nature” by Oxford Dictionary. Revenue is the money a company receives in payment for its products or services. Revenue is not the profit, but instead, it is the total amount of money earned by an organization before deducting any expenses or taxes. Revenue has a significant impact on the profit. It is important to create the widest possible difference between the cost and the revenue of the business. “All administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.” Healthcare Financial Management Association (HFMA). Healthcare revenue cycle involves several steps such as patient registration, insurance verification & eligibility, medical documentation, chart review & coding, claim submission, payment posting, and accounts receivable & collections. Any incorrect or erroneous entry at any point in the revenue cycle can turn it into a vicious cycle. The farther an erroneous entry moves into the revenue cycle the more difficult it becomes to trace and rectify it.
INTRODUCTION
Revenue Cycle Management (RCM) in healthcare is the process of managing claims process, payment, and revenue generation. RCM in healthcare helps a medical practice to increase the revenue by proper claim management. If the claims are paid partly or if it is paid after a long period of time, then resources from the accounts receivable and collection department need to be utilized in order to get the claim settled. This delay in claim payment and consecutive follow-ups from the accounts receivable and collection department would generally have a negative effect on the revenue cycle. RCM unifies the business and clinical sides of healthcare by coupling administrative data, such as a patient’s name, insurance provider and other personal information, with the treatment a patient receives and their healthcare data.
KEY PLAYERS IN REVENUE CYCLE MANAGEMENT OF HEALTHCARE
Time management and productivity play key elements in the healthcare RCM.
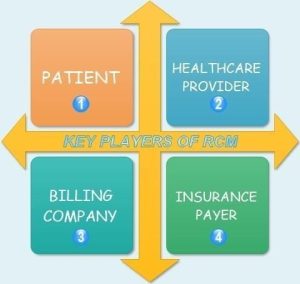
There are four key players involved in the Revenue Cycle Management of healthcare system namely:
- Patient
- Healthcare provider
- Billing company
- Insurance payer
It is imperative that all the four players align their goals and work in tandem so that the revenue cycle process runs smoothly.
STAGES IN REVENUE CYCLE MANAGEMENT
Due to the automation of the revenue cycle process, today, computers have replaced the typewriters used by the medical transcriptionists, servers have replaced the file cabinets used to store the medical records documentation, electronic dictionaries and software have replaced the traditional dictionaries and coding manuals, and electronic data interchange (EDI) has replaced the US Postal Service to send claims. This automation has led to reduction in the billing cycle period as well as decrease in the number of errors.
A medical practice’s choice of practice management software (PMS) should be largely centered on how the RCM needs to be implemented. One other important reason to develop an efficient revenue cycle is working on claim denials and claim rejections. Maximum number of these claims is denied for trivial reasons and RCM helps to identify those insignificant cause and root it out so that lesser amount of denial occurs thereby increasing the medical practice revenue. Proper revenue cycle management works on each and every stage of the revenue cycle to increase the payments and collections while decreasing the write-offs.
In a nutshell, we can describe the revenue cycle as consisting of three stages:
- Preservice
- Service Stage.
- Post service Stage.
- Preservice Stage: Preservice stage consists of all the activities prior to the patient’s encounter with the healthcare provider or in other word prior to the patient receiving any kind of healthcare service. The patient’s call to the medical practice, gathering of the information – patient’s demographic and patient’s insurance, verification of the insurance information, real-time eligibility, authorization information, and financial position of the patient – payments due in the past all these form part of the preservice
- Service Stage: Service stage is the actual point where the patient receives the healthcare service for the medical ailment. This stage is the core activity stage of the revenue cycle The patient visiting the clinic/hospital, the patient’s encounter with the healthcare provider (provider’s examination, diagnosis, and treatment plan), medical transcription, medical coding, and medical billing are part of the service stage. The service stage consumes most of the resources of any medical practice.
- Post service Stage: Post service stage is the last stage of the RCM after the healthcare service to the patient has been delivered.
Claim submission, patient statement/invoice, payment posing, accounts receivable, working on denials and appeals, write-offs and refunds, and assigning to collection agency form part of the post service stage.
To summarize, the three stages of RCM is comprised of all the administrative, clinical, and financial functions of a medical practice.
HEALTHCARE REVENUE CYCLE PROCESS
Generally, a revenue cycle process involves the following ten steps:
- Patient Verification & Scheduling
- Patient and Provider Encounter
- Medical Transcription
- Charge Entry
- Medical Coding
- Claim Submission
- Payment Posting
- Accounts Receivable
- Write off, Refund, & Collections
- Closing of Account
REVENUE CYCLE MANAGEMENT SYSTEM
A desirable revenue cycle management solution should have the capability to shorten the billing cycle by assisting the medical billing department in producing more and more clean claims and fewer and fewer write-offs. It is imperative to choose a good revenue cycle management solution as it has the capacity to make or break a medical practice.
Some of the basic features of revenue cycle management solutions are as follows:
- Real-Time Data
- Ability to Integrate and Upgrade
- Security
- Hybrid (Professional and Institutional)
- Patient Focused
- Mobility
a. Real-Time Data:
A revenue cycle management solution should be able to generate real-time data instantly and make them available for use by the front-office staff, back-office staff, and the providers. There are typically three types of real-time data required in the revenue cycle, viz, Real-time eligibility (Used by the front-office staff) Real-time report generation (Used by the back-office staff)Real-time clinical information (Used by the providers) These detailed reports are used for effective decision making that would help in proper management all aspects of patient’s care such as clinical, financial, and administrative.
b. Ability to Integrate and Upgrade:
In this dynamic environment where rules are constantly changing, the medical practice should have a revenue cycle management system that offers great level of flexibility and scalability to adapt to changing business rules at any time in the future. The integration of the RCM system with other applications used in the hospital will allow for easy data sharing across the healthcare delivery system, because a blend of heterogenous systems will not only make it difficult to identify problem-causing areas but also make it extremely difficult to generate reports. Therefore, an RCM system should be dynamic with ability to integrate with other application as well as to be upgraded as and when needed.
c. Security:
An RCM system should have a robust and comprehensive security feature. Care should be taken to ensure that the system is HIPAA certified as it would play a critical role in determining the HIPAA compliance process of the medical practice. It should have enough administrative, physical, and technical safeguards to prevent the misuse of any protected health information. Features such as role-based access control, unique username and password, data encryption, etc., are essential for any RCM. Role-based access control is restraining an individual to access only those files and folders which are essential to perform the individual’s job duties. Level access is granted strictly to only minimum required data depending on the employee’s job responsibilities.
d. Patient Focused:
Lately, patients have become more aware and want to actively participate in the clinical and financial decisions regarding their healthcare. If patients on a regular basis can track their ongoing healthcare progress both in terms of clinical and financial aspects, it would greatly help in making an informed decision and would help in developing a positive relationship between the patient and the provider. HIPAA encourages utilizing healthcare technologies to increase patient involvement in order to be eligible for the incentive program set up by Medicare and Medicaid. The patient’s involvement into joint decision making will also healthcare providers cut costs on several grounds such as registration and scheduling (by engaging online pre-registration forms), financial counseling (by allowing the patient to calculate an estimate of patient’s responsibility), collections (by electronic fund transfer from patient’s account), etc.
IMPLEMENTATION OF REVENUE CYCLE MANAGEMENT SYSTEM
An RCM system sporting the above features would cause a positive impact on the revenue cycle managing the financial aspects as well as clinical aspect of care and at the same time changing towards a better care coordination. Implementation of a wrong RCM system would impact the hospital’s financial stability and affect future performance. One fundamental question that needs to be kept in mind before zeroing down on an RCM system is to review the need and budget of the medical practice/hospital and select a system that fits within the hospital’s budget as well fulfills the current and future needs.
CONCLUSION:
Our reimbursements on claims filed, and therefore the cash paid out of pocket by patient’s area unit the idea of your revenue cycle. The extent to that you effectively manage your payment processes associate degree have a handle on grouping payments that are unit overdue is an indicator of your practice’s money health. Whereas this is smart intuitively, the actual execution of effective revenue cycle management could be a challenge to the common follow owner. Not solely is the U.S. healthcare payment system designed to figure against you, but you’ll otherwise lack the time, experience, or internal systems to confirm that you simply get paid the most you’re owed as quickly as doable. Having applicable technology, adequate progress, and practiced charge personnel area unit vital steps on the trail toward a prosperous and economical follow. A lot of that you simply will integrate these assets into your charge performance, the stronger influence you’ll be able to have over money outcomes. Practices that lack in these key areas may have to gauge if they’re candidates for outsourcing.
References:
- https://www.techtarget.com/searchhealthit/definition/revenue-cycle-management- RCM
- https://www.carecloud.com/continuum/what-is-revenue-cycle-management-rcm/
- https://www.greenwayhealth.com/knowledge-center/greenway-blog/what- revenue-cycle-management
- https://www.collaboratemd.com/blog/the-steps-and-benefits-of-revenue-cycle- management/
- https://en.wikipedia.org/wiki/Revenue_cycle_management
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 


 Virtual Medical Assistants
Virtual Medical Assistants



