Summarize this blog post with:
How Does Accurate Medical Coding Affect Patient Care in Connecticut?

Accurate medical coding isn’t just about ensuring correct billing—it plays a direct role in patient care. In Connecticut, healthcare providers rely on precise coding to streamline treatment plans, ensure compliance, and improve financial stability. Without proper coding, errors can lead to claim denials, delays in care, and even patient misdiagnosis. This is where revenue cycle management BPO services become essential, helping providers maintain accuracy and efficiency in medical documentation.
The Connection Between Medical Coding and Patient Care
Medical coding is the backbone of healthcare administration, ensuring that every diagnosis, treatment, and procedure is accurately documented. These codes (ICD-10, CPT, and HCPCS) serve multiple functions, from insurance claim processing to tracking public health trends. However, even minor coding errors can disrupt patient care, delay reimbursements, and create compliance risks. This is why revenue cycle management BPO services are essential for healthcare providers in Connecticut, improving coding accuracy and financial stability.
1. Faster and More Efficient Treatment Plans
Accurate coding allows healthcare providers to access a patient’s full medical history quickly. This enables physicians to make informed decisions without delays caused by missing or incorrect information. For example, a cardiologist treating a heart condition needs precise records of past procedures and medications. Inaccurate codes can lead to redundant tests or incorrect prescriptions, delaying the best course of action. By leveraging revenue cycle management BPO services, healthcare facilities can ensure coding accuracy, reducing errors that slow down treatment.
2. Improved Insurance Approvals and Reduced Claim Denials
One of the biggest challenges for healthcare providers and patients is insurance claim denials. Many denials result from coding errors, such as incorrect modifiers, mismatched diagnoses, or missing documentation. When Connecticut providers utilize revenue cycle management BPO services, they benefit from coding accuracy that speeds up approvals, ensuring patients receive timely treatments without financial obstacles. Fewer claim denials mean improved cash flow for providers and a smoother experience for patients.
3. Better Compliance and Reduced Legal Risks
Healthcare facilities in Connecticut must adhere to strict state and federal regulations, including HIPAA and Medicare guidelines. Inaccurate coding can trigger audits, financial penalties, and even fraud investigations. By partnering with revenue cycle management BPO services, healthcare organizations can ensure compliance, reducing the risk of costly legal issues and maintaining a high standard of patient care.
4. More Accurate Public Health Data
Medical coding plays a significant role in shaping public health policies. State and federal agencies rely on coded data to track disease outbreaks, assess healthcare trends, and allocate resources effectively. However, errors in coding can distort public health data, leading to misinformed policy decisions. Connecticut providers using revenue cycle management BPO services can improve the accuracy of this data, contributing to better healthcare planning and disease prevention efforts.
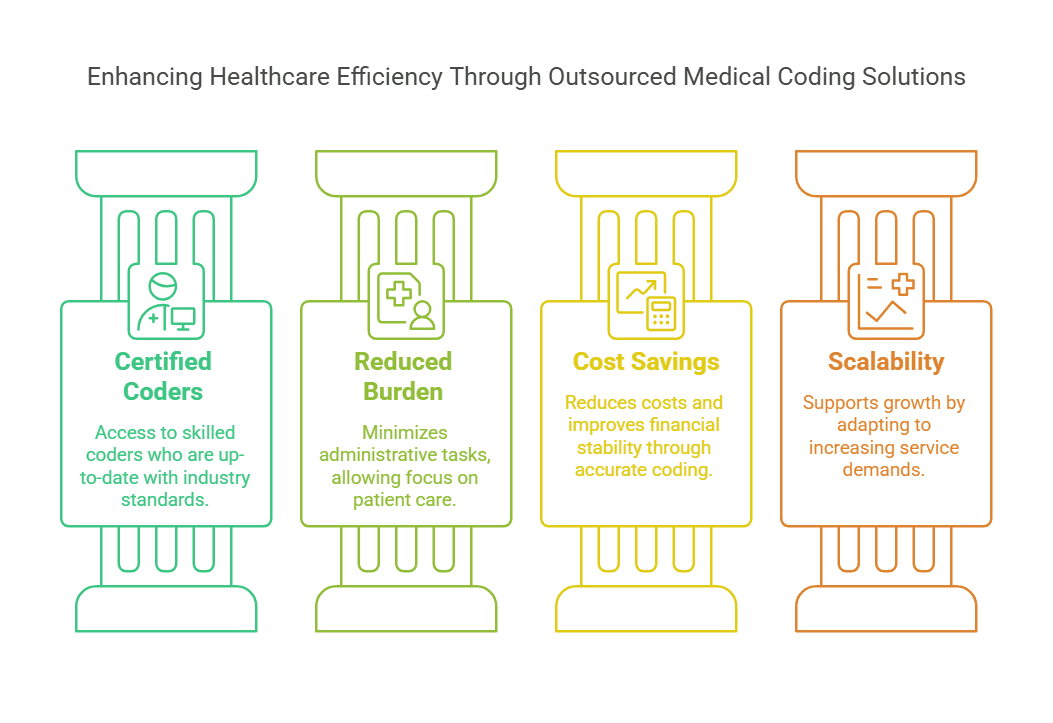
Why Healthcare Providers in Connecticut Should Consider Outsourcing Medical Coding
Many healthcare facilities struggle with in-house coding due to staffing shortages, high error rates, and evolving industry regulations. Revenue cycle management BPO services offer a cost-effective solution, providing experienced coders who specialize in accuracy, compliance, and efficiency. Here’s why outsourcing is a smart choice:
1. Access to Certified Medical Coders
Professional outsourcing firms employ AAPC- and AHIMA-certified coders who stay up to date with coding changes. Connecticut providers benefit from expert coders without the need for in-house training.
2. Reduced Administrative Burden
Hospitals and private practices often struggle with administrative overload. Outsourcing coding allows providers to focus on patient care rather than paperwork.
Frequently Asked Questions
1. What are the most common medical coding errors?
Common errors include incorrect procedure codes, mismatched diagnoses, missing modifiers, and outdated codes. These mistakes can lead to claim rejections or delays in patient treatment.
2. How does medical coding impact healthcare revenue?
Accurate coding ensures timely reimbursement from insurance providers. Errors lead to claim denials, rework, and lost revenue, affecting the financial health of healthcare organizations.
3. Why should healthcare providers outsource medical coding?
Outsourcing ensures accuracy, compliance, and efficiency. It reduces administrative workload, lowers costs, and improves revenue cycle management.
4. What is the difference between CPT and ICD-10 codes?
CPT codes describe medical procedures and services, while ICD-10 codes classify diseases and health conditions. Both are essential for accurate billing and patient records.
5. How do revenue cycle management BPO services help with medical coding?
They provide certified coders, advanced technology, and quality control measures to minimize errors, ensuring smooth claim processing and better patient care.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services,
please contact Staffingly, Inc. at (800) 489-5877
Email : support@staffingly.com.
About This Blog : This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!

 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



