On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesMEDICATION REVIEW PROCESS BY CLINICAL PHARMACIST IN HOSPITALIZED PATIENTS – A REVIEW

AUTHOR: P.P.PUSHPALATHA
ABSTRACT :
The medication Review process is the process of communication between the patient and the pharmacist to promote the safe and effective use of medications. Medication review services are mostly recommended for patients who are taking several medications at the same time. There are different types of medication reviews namely medication standard, medication pharmacist consultation, and medication follow-up. The medication review process mainly focuses on Medication reconciliation and medication discrepancy. Medication reconciliation targets preventing adverse drug events and it remains a top patient safety priority and also an effective strategy for preventing ADE’S. Reconciliation aims to eliminate undocumented intentional discrepancies and unintentional discrepancies by reconciling all medications at all interfaces of care. In this, mostly a discharge medication discrepancy shows a very significant role and during the discharge process, an electronic discharge medications list is prepared and printed from the electronic health record. The electronic medication administration record and the medication list from the patient history were obtained on admissions. Finally, the detected discrepancies were documented for each patient with the patient’s demographic details and clinical data. The study mainly confirms that medication reconciliation is a critical component for the safe and effective patient care of hospitalized patients. Medication discrepancies at hospital discharge are common and in most cases of major potential harm. Having qualified clinical pharmacists review the medication process, reconciliation and discrepancies help to improve medication use safety and reduce medication errors.
KEYWORDS: Medication reconciliation, Medication discrepancy, adverse drug events, medication errors.
- INTRODUCTION :
The medication review’s overall aim is to improve the quality, safety, and appropriate use of medicines and prevent any medication-related problems, and optimize medication use in collaboration with GPs, medical practitioners, other healthcare professionals, and patients. the process is patient-centered. Medication reviews form the foundation of national policies and guidelines associated with medication optimization strategies and intervention studies. These remunerated services include Medication Therapy Management and Medication Regimen Review in the United States of America (USA), Residential Medication Management Review (RMMR) and Home Medicines Review (HMR) in Australia, Medicines Use Review in the United Kingdom, and MedsCheck in Canada.
Future of medication use reviews
In the coming future, technology has improved medication review as a tool for healthcare. A systematic review has shown how technology can reduce costs due to time savings and improve individual health outcomes and safety.
Adopting technology in medication reviews:
The use of technology is being implemented in healthcare in various ways. The use of mobile devices and apps for healthcare professionals that have provided many benefits, including increased access to point-of-care tools which are proven to support improved clinical decision-making and patient outcomes. Telepharmacy” is defined as using communication technology and electronic information for the provision and support of comprehensive pharmacy services particularly when distance separates participants. Medication reviews could be ‘integrated’ with other clinical information systems such as electronic health records, rather than being ‘stand-alone manual processes’
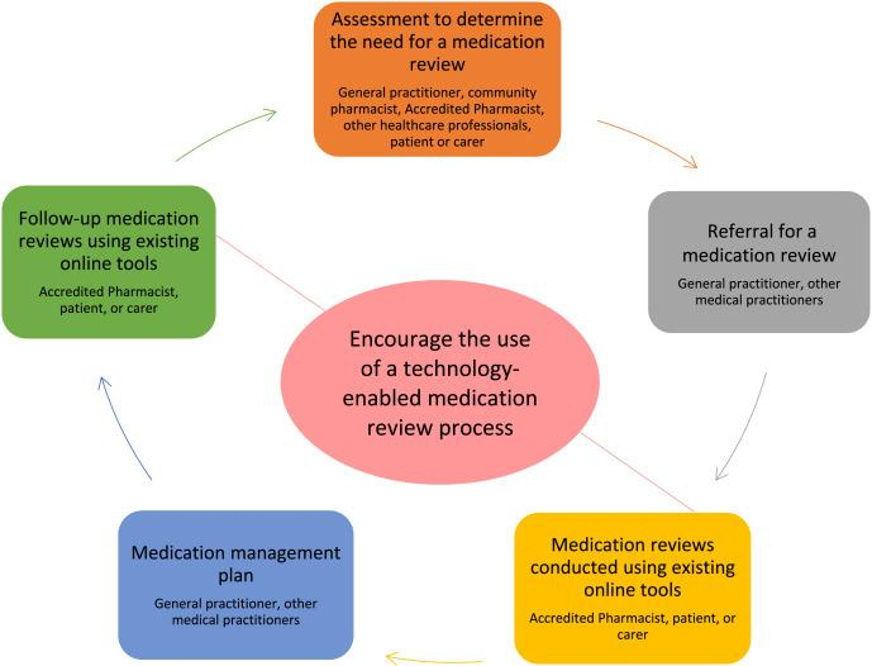
Fig-1: A general overview of the medication review process in Australia (adapted from the Guidelines for comprehensive medication management reviews 2020)
Systematic medication reviews have been introduced as a procedure to optimize medication use and reduce Medication-related problems. There are different types of medication reviews, they are :
- Prescription review
- Compliance and concordance review
- Clinical medication review
- Prescription review: The prescription review is defined as the process of evaluating and standardizing prescription writing and determining the suitability of the clinical use of drugs according to the relevant regulations and technical specifications.
- Compliance and concordance review:
Compliance:
Compliance in medicine refers to the ability of an organ to distend in response to applied pressure. In physics, compliance refers to the property of a material undergoing elastic deformation or (of a gas) changing in volume when subjected to an applied force. Compliance is a restrictive, authoritarian term that implies obedience to doctors’ orders.
Concordance:
The term refers to the deep knowledge of the relationship and to the achievability of examining crucial questions regarding the patient’s lifestyle. The concept of medication concordance entails all practicing family physicians who interact with the patients in their day-to-day clinical practice. The entire concept revolves around patient–doctor relationship. Concordance takes into account and gives due importance to the health beliefs of the patient. It seeks to establish a collaborative “therapeutic alliance” aimed at fulfilling the aspirations and expectations of both patient and doctor. Concordance is a dynamic process, achievable but requiring a set of approaches to patient therapy and management different from the ones currently being practiced in medicine. There is prevailing incoherence between attempts to align individualized care with a predetermined outcome-based clinical practice. Concordance, in contrast, is an end in itself, more coherent with shared care than adherence or compliance, but rejected by many guideline developers of various nations because of its complexity.
- Clinical medication review:
Clinical medication reviews are comprehensive,
confidential checks held by doctors on the medication used by patients. These reviews have several objectives. These reviews are best for patients taking multiple medications for long-term chronic conditions. Medication reviews are also crucial for people to withstand various illnesses, whether related or unrelated to each other. To perform the check, the doctor will ask the patient to come in with all current prescriptions. From there, the doctor will ask a series of questions, including:
- If the patient is using the medication as directed.
- How the medicine makes the patient feel.
- If there are any concerns about side effects.
- If the patient is taking non-prescribed herbs, drugs, or supplements.
A final review of the medication helps the doctor determine if anything needs to be changed.
Clinical Pharmacists also have the sovereignty to discuss and perform medication reviews. A community or hospital pharmacist has extensive knowledge of medication and each drug’s effectiveness. Medication reviews have now become a key task for pharmacists, particularly in the community. Since pharmacists are easily accessible, a patient with multiple prescriptions can have a review with little hassle. Relying on a pharmacist has a range of other benefits
- MEDICATION RECONCILIATION :
The implementation of the medication reconciliation process to improve patient safety by identifying unintended medication discrepancies, especially at transitions of care. medication reconciliation remains a critical patient safety activity that is supported by different international organizations to optimize patient medication safety at transitions of care.
Various medication reconciliation interventions have been evaluated to identify medication reconciliation best practices.
The cornerstone for successful medication reconciliation is creating the best possible accurate medication list by using a systematic approach based on a patient/carer interview and a variety of other medication sources such as prescription bottles, discharge medication orders, or pharmacy records.
Medication reconciliation is an important component of the care of hospitalized patients and their safe transition.
An extensive list of medications should include all prescription medications, herbals, vitamins, nutritional supplements, over-the-counter drugs, vaccines, diagnostic and contrast agents, radioactive medications, parenteral nutrition, blood derivatives, and intravenous solutions. All medications and supplements should be part of a patient’s medication history and included in the reconciliation process.
Admission and discharge information transfer steps
In simplified terms, six steps—which are remarkably similar at all three IDSs studied—are used to gather, organize, and communicate clinical information at admission and discharge.
At admission—
- the admitting physician writes admitting medication orders;
- nurses document the patient’s historical medications; and
- inpatient pharmacists create a medication administration record (MAR).
At discharge—
- the discharging physician develops discharge instructions for the patient;
- nurses educate the patient about the discharge instructions; and
- the new medication regimen is transmitted to the follow-up physician in a discharge summary.
Research evidence:
Medication reconciliation studies have focused on the accuracy of the medication history during various transitions: ambulatory to an acute care inpatient setting, skilled nursing facility to an acute care inpatient setting, inpatient acute care setting to the skilled nursing facility, inpatient acute care setting to discharge, inpatient floor to the intensive care unit (ICU), and ICU to discharge. Little research has focused on outcomes related to the prevalence of errors resulting from a lack of or incomplete patient medication lists.
Medication reconciliation is the process of comparing a patient’s medication orders to all of the medications that the patient has been taking. This reconciliation is done to avoid medication errors such as omissions, duplications, dosing errors, or drug interactions. It should be done at every transition of care in which new medications are ordered or existing orders are rewritten. Transitions in care include changes in setting, service, practitioner, or level of care. This process comprises five steps:
- develop a list of current medications;
- develop a list of medications to be prescribed; (3) compare the medications on the two lists; (4) make clinical decisions based on the comparison; and (5) communicate the new list to appropriate caregivers and the patient.
Errors prevented by medication reconciliation include inadvertent omission of therapy, prescribing a previously ceased medicine, the wrong drug, dose, or frequency, failure to recommence withheld medicines, and duplication of therapy after discharge. Implementing formalized medication reconciliation at admission, transfer, and discharge reduces medication errors by 50–94%and reduces those with the potential to cause harm by over 50%. The process is also associated with improved patient outcomes and a tendency for reduced readmissions.
1. Develop a list of a patient’s current medications
The first step is perhaps not only the most important but also the most challenging of the medication reconciliation steps: documenting all a patient’s current medications. If even a single medication or critical detail about a medication (e.g., dosage, frequency, route of administration) is omitted from this list, the risk of an adverse drug event increases, and the ability to effectively and appropriately complete the remaining medication reconciliation steps decreases.
Here are just some of the reasons why developing a current medication list can prove so difficult:
- Patients are taking more medications than ever. As the number of medications grows, so does a patient’s ability to recall all their medications and associated details. Consider that a study published in 2012 showed that only 36% of patients were able to provide a medication list that matched their pharmacy-prescribed drugs. This figure has likely declined as medication regimens have continued to grow in complexity.
- Patients are taking more non-prescription drugs, including over-the-counter drugs, vitamins, herbals, and dietary supplements. These should be included on a patient’s current medication list.
- Patients often see multiple specialists who prescribe medications, so there may not be a single provider source with a current medication list.
- Patients often fill medications at multiple pharmacies, which may now include those operating online. A pharmacy is only likely to have records for those medications that were filled there.
- A drug may have multiple names associated with it (i.e., brand, generic, chemical). Some drug names can be easily confused with others.
- Cognitive impairment issues can make medication regimen recollection by patients more challenging.
- Electronic health record (EHR) systems are often missing data from providers and facilities not connected to that EHR.
2. Develop a list of medications to be prescribed
This step may seem easy, but that brings with it a potential for mistakes. A false sense of confidence can encourage the rushed completion of responsibilities and corner-cutting. As an Academy of Managed Care Pharmacy article notes, these are just some of the ways preventable prescribing errors occur:
- Illegible handwritten prescriptions
- Incorrect selection of drug or dose
- Oral transmission of prescriptions can lead to sound-alike name confusion
- Drugs with similar-looking names can be incorrectly dispensed when prescriptions are handwritten
3. Compare the medications on the lists
This is essentially the “reconciliation step” in the medication reconciliation process. The comparison of the lists helps ensure discrepancies can be avoided and red flags can be identified, such as omitted medications, therapeutic duplications, dosing errors, drug-drug interactions, and drug-disease interactions.
Considering that any of these issues can put a patient’s health and wellness at risk, why is this step sometimes missed or not completed appropriately? Some of the top reasons include the following:
- Time: As we previously noted in our medication reconciliation guide, “Clinicians sometimes spend less than 15 minutes with a patient during an appointment and can lack the time necessary to perform proper medication reconciliation.”
- Unclear roles and responsibilities: If there is confusion about who is supposed to perform medication reconciliation, the likelihood that it will occur decreases.
- Lack of timing clarity: Similarly, confusion about when medication reconciliation must be performed (e.g., medication reconciliation post-discharge) increases risks.
- Poor communication: When a patient or a patient’s information is not effectively handed off at transition points, errors are more likely to occur. This can include a failure to pass along new medication orders that would then necessitate medication reconciliation.
4. Make clinical decisions based on the comparison
This is another one of the medication reconciliation steps that can suffer due to time issues. When those performing medication reconciliation lack the adequate time and resources to effectively complete the process, decision-making is likely to be rushed or cut short.
One aspect of medication management that can be negatively affected concerns efforts around deprescribing, which, as we previously noted, “… has become one of the most effective ways to safely decrease inappropriate and unnecessary polypharmacy.”
Unfortunately, as a Health Affairs article states, “In many cases, medication reconciliation has devolved into a box-checking exercise to comprehensively catalog all medications a patient is taking, but the process may not make efforts to decrease the number of medications or stop potentially harmful drugs.”
5. Communicate the reconciled medication list to the patient and appropriate caregivers
If the preceding four medication reconciliation steps are completed, this final step is typically completed in some fashion. At a minimum, a patient is usually provided with the revised medication list. But even this can experience problems. They include the following:
- Providers may rush their review and discussion of the list with the patient, potentially stifling a patient’s willingness to ask questions.
- A rushed discussion may cause a provider to miss warning signs of an increased likelihood of medication non-adherence.
- A rushed review may also lead to a missed opportunity for a discussion around medication adherence. As we previously noted, “Medication reconciliation and adherence are not divorced discussions, and the additional few minutes can make a huge difference in the patient’s outcome.”
MEDICATION DISCREPANCY:
The terms intentional and unintentional were often used in the literature to describe types of medication discrepancies. More than 50% of hospitalized patients experience one or more unintentional medication discrepancies (UMDs), defined as unexplained differences in medication regimens across different sites of care, with some having the potential for significant harm. Medication reconciliation (MedRec) reduces the risk of UMDs and harmful adverse drug events that increase hospitalization costs and length of stay. MedRec is the process of “creating the most accurate list possible of all medications a patient is taking and comparing that list against the physician’s admission, transfer, and/or discharge orders, intending to provide correct medications to the patient at all transition points within the hospital”
Medication discrepancy at discharge :
A discharge medication discrepancy was defined as any difference identified between the medications listed on the discharge prescription and the medications list from the patient history, Medication Administration Record (MAR), or home medications list.
- An intentional discrepancy is one that the prescriber intentionally made to meet the patient’s need with documentation of the intended change in the clinical record, while an unintentional discrepancy is one that was accidentally made by the physician or pharmacist and/or lacked documentation in the clinical records. The prescriber was contacted in case of uncertainty. Two investigators further classified independently unintentional discrepancies into major, moderate, and minor. The major discrepancy is the one detrimental to the patient’s outcome and will usually result in significant harm to the patient if the current practice continued; including poor disease control, worse quality of life, increased symptoms, worse survival, and/or hospitalization. The moderate discrepancy is the one that could have an undesirable effect on the patient’s outcome. The minor discrepancy is the one that would probably not affect the patient’s outcome. Medication discrepancies occur commonly on hospital discharge. Understanding the type and frequency of discrepancies can help clinicians better understand ways to prevent them. Structured medication reconciliation may help to prevent discharge medication discrepancies.
- Each unintentional medication discrepancy was then classified by drug class (according to the Anatomical Therapeutic Chemical Classification System—ATC) and type of unintentional medication discrepancy (e.g., omission of medication, change of medication, extra medication, or difference in dose or dosing frequency).
- Unintentional discrepancies were classified into 3 main categories. Drug discrepancies included omission or commission; therapeutic duplication (ie, both formulary substitution and original home medication included on prescription), inappropriate route, and formulary substitution not restored to original home medication. Dose discrepancies included incorrect dose (eg, tablet strength that is not available). The category of incomplete prescriptions included those with missing limited use (LU) code (where applicable), misspelled drug name, omission of formulation, omission of dose, omission of frequency, quantity missing on medications meant to be filled at a community pharmacy, and providing repeats on narcotic drugs
- CONCLUSION: A Clinical pharmacist’s primary concern is the safety of the patient. If there are medicine or supplement combinations with dangerous side effects, the pharmacist can remove or replace the medication immediately. Furthermore, if something reduces the drug’s effectiveness, the doctor can make the necessary adjustments. The goal of medication reconciliation is to obtain and maintain accurate and complete medication information for a patient and use this information within and across the continuum of care to ensure safe and effective medication use. Currently, medication reconciliation has become a standard healthcare practice recommended by the WHO and many countries. Few studies have discussed medications as a risk factor for hospital readmission, and some studies have examined post-discharge follow-ups with pharmacist involvement as well. However, this study focused specifically on the impact that medication discrepancies have on discharge rates within 30 days of discharge. One study suggested that the quality of medication reconciliation may be associated with the risk of readmission. Finally, I conclude this review article as medication review, medication reconciliation, and medication discrepancies are very important in every hospital which is demonstrated by clinical pharmacists and should improve in each hospital.
REFERENCES :
- Blenkinsopp, A., Bond, C., & Raynor, D. K. (2012). Medication reviews. British Journal of Clinical Pharmacology, 74(4), 573-580. https://doi.org/10.1111/j.1365-2125.2012.04331.x
- Thiruchelvam, K., Byles, J., Hasan, S. S., & Kairuz, T. (2022). Innovating medication reviews through a technology-enabled process. Research in Social and Administrative Pharmacy, 18(4), 2700-2705. https://doi.org/10.1016/j.sapharm.2021.07.019
- Pharmaceutical Society of Australia
Guidelines for comprehensive medication management reviews
accessed on https://www.ppaonline.com.au/wp-content/uploads/2020/04/PSA-Guidelines-for-Comprehensive-Medication-Management-Reviews.pdf (2020), Accessed 10th Jun 2021 Google Scholar
4. Xu, F., Yin, J., & Zeng, S. (2020). The practice of prescription review mode based on data mining in hospitals. Annals of Translational Medicine, 8(14). https://doi.org/10.21037/atm-20-3933
5.Almanasreh, E., Moles, R., & Chen, T. F. (2016). The medication reconciliation process and classification of discrepancies: a systematic review. British Journal of Clinical Pharmacology, 82(3), 645-658. https://doi.org/10.1111/bcp.13017
6.Kreckman, J., Wasey, W., Wise, S., Stevens, T., Millburg, L., & Jaeger, C. (2017). Improving medication reconciliation at hospital admission, discharge, and ambulatory care through a transition of the care team. BMJ Open Quality, 7(2). https://doi.org/10.1136/bmjoq-2017-000281
7. Barriers Associated with Medication Information Handoffs
- Bruce Bayley, Lucy A. Savitz, Glenn Rodriguez, William Gillanders, and Steve Stone.
- 5 medication reconciliation steps to complete at every care transition-S.Micheal Ross MD, MHA,MAY 26,2021
- Al-Rashoud, I., Al-Ammari, M., Al-Jadhey, H., Alkatheri, A., Poff, G., Aldebasi, T., AbuRuz, S., & Al-Bekairy, A. (2017). Medication discrepancies were identified during medication reconciliation among medical patients at a tertiary care hospital. Saudi Pharmaceutical Journal: SPJ, 25(7), 1082-1085. https://doi.org/10.1016/j.jsps.2017.05.004
- Delate T., Chester E.A., Stubbings T.W., Barnes C.A. Clinical outcomes of a home-based medication reconciliation program after discharge from a skilled nursing facility. 2008;28:444–452. [PubMed] [Google Scholar]
- Grimes T.C., Duggan C.A., Delaney T.P., Graham I.M., Conlon K.C., Deasy E., Jago-Byrne M.C., O’Brien P. Medication details documented on hospital discharge: a cross-sectional observational study of factors associated with medication non-reconciliation. J. Clin. Pharmacol. 2011;71:449–457. [PMC free article] [PubMed] [Google Scholar]
- Hammour K.A., Farha R.A., Basheti I. Hospital pharmacy medication reconciliation practice in Jordan: perceptions and barriers. Eval. Clin. Pract. 2016 [PubMed] [Google Scholar]
- Herrero-Herrero J.I., Garcia-Aparicio J. Medication discrepancies at discharge from an internal medicine service. J. Int. Med. 2011;22:43–48. [PubMed] [Google Scholar]
- InstituteforHealthcareImprovement, 5 Million Lives Campaign. 2006. <www.ihi.org/MedicationReconciliationReview>(accessed 2016, March 16)
- Joint Commission National Patient Safety Goals. 2012. <http://www.jointcommission.org/assets/1/6/NPSG_Chapter_Jan2012_HAP.pdf>(accessed 2016, March 15)
- Kaboli P.J., Hoth A.B., McClimon B.J., Schnipper J.L. Clinical pharmacists, and inpatient medical care: a systematic review. Intern. Med. 2006;166:955–964. [PubMed] [Google Scholar]
- Karapinar-Carkit F., Borgsteede S.D., Zoer J., Smit H.J., Egberts A.C., van den Bemt P.M. Effect of medication reconciliation with and without patient counseling on the number of pharmaceutical interventions among patients discharged from the hospital. Pharmacother. 2009;43:1001–1010. [PubMed] [Google Scholar]
- Murphy E.M., Oxencis C.J., Klauck J.A., Meyer D.A., Zimmerman J.M. Medication reconciliation at an academic medical center: implementation of a comprehensive program from admission to discharge. J. Health Syst. Pharm. 2009;66:2126–2131. [PubMed] [Google Scholar]
- Nickerson, A., MacKinnon, N.J., Roberts, N., Saulnier, L., 2005. Drug-therapy problems, inconsistencies, and omissions are identified during a medication reconciliation and seamless care service. Healthc Q. 8 Spec No, pp. 65–72. [PubMed]
- Wong, J. D., Bajcar, J. M., Wong, G. G., Alibhai, S. M., Huh, H., Cesta, A., Pond, G. R., & Fernandes, O. A. (2008). Medication Reconciliation at Hospital Discharge: Evaluating Discrepancies. Annals of Pharmacotherapy. https://doi.org/10.1345/aph.1L190
- Compliance and concordance–ReNue pharmacy
11.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688-1698. doi:10.1001/jama.2011.1515
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 


 Virtual Medical Assistants
Virtual Medical Assistants



