On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
How Prior Authorization Works in Staten Island, NYC Medicare Advantage Plans?
Understanding prior authorization (PA) is essential if you’re a healthcare provider or a patient using Medicare Advantage plans in Staten Island, NYC. This process ensures that specific medical treatments or procedures are both necessary and covered by insurance. While it can feel overwhelming, this article will break down the steps, challenges, and solutions to make the process easier. Let’s explore how prior authorization works and how you can manage it more effectively.
What Is Prior Authorization?
Prior authorization is the process of getting approval from an insurance provider before a service, procedure, or medication is administered. For Staten Island residents on Medicare Advantage Plans, this step is required for certain treatments to confirm they are medically necessary.
Common services needing prior authorization include:
- Diagnostic imaging like MRIs or CT scans.
- Expensive specialty medications.
- Elective or complex surgeries.
- Durable Medical Equipment (DME).
Prior authorization acts as a safeguard, but it can also slow down the care process if not managed well.
Why Is Prior Authorization Important?
Prior authorization serves several purposes:
- Cost Management: It ensures that healthcare resources are used effectively.
- Patient Safety: Helps avoid unnecessary treatments or medications.
- Quality of Care: Encourages providers to follow evidence-based medical practices.
For healthcare providers in Staten Island, managing prior authorization can be time-consuming. It involves significant administrative work, delays in care, and coordination between providers and insurers.
How Does the Prior Authorization Process Work?
Here’s how the prior authorization process typically works for Medicare Advantage Plans in Staten Island:
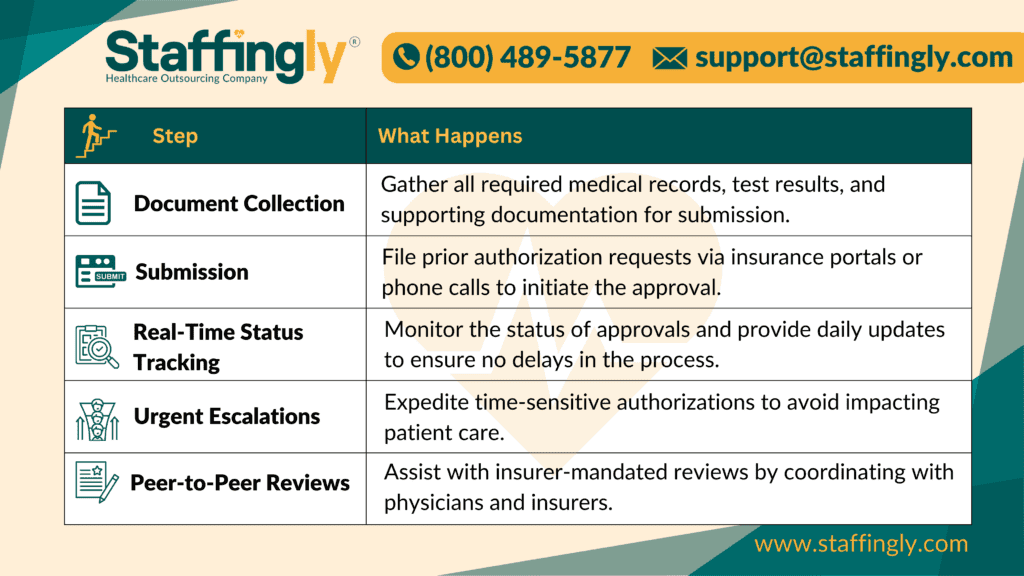
The entire process requires careful attention to detail, and any errors can lead to denials or delays in patient care.
Challenges Providers Face in Staten Island
Healthcare providers in Staten Island face several challenges when handling prior authorization:
- Delays in Treatment: Approval processes can take days or even weeks.
- Administrative Overload: Significant time and resources are spent managing documentation, submissions, and follow-ups.
- High Denial Rates: Errors or missing documentation often lead to denials, requiring additional time to appeal.
These challenges can take a toll on your practice, staff, and patients. That’s where outsourcing can help.
How Staffingly, Inc. Can Help
Managing prior authorization doesn’t have to be a headache. Staffingly, Inc. offers end-to-end support to streamline the process and reduce the burden on your team. Here’s how:
1. Comprehensive Document Management
Staffingly collects and organizes all necessary documents, ensuring every submission is complete and accurate.
2. Fast and Accurate Submissions
Our team submits prior authorization requests promptly via insurance portals or phone calls, reducing delays.
3. Real-Time Tracking and Updates
We monitor approvals in real time, providing regular updates so you’re never left wondering about the status of a request.
4. Handling Urgent Requests
For time-sensitive procedures, we fast-track urgent authorizations to ensure care is not delayed.
5. Denial Appeals
If an authorization is denied, we handle the appeals process with detailed resubmissions to avoid disruptions.
With Staffingly, healthcare providers can save time, reduce administrative stress, and focus on delivering excellent patient care.
Real-Life Example: Staten Island Clinic Success
Let’s look at an example: A clinic in Staten Island was struggling with prior authorization delays for Medicare Advantage patients needing MRIs. The process was overwhelming their administrative team and causing frustration for patients.
After partnering with Staffingly, the clinic experienced:
- 40% faster turnaround times for prior authorizations.
- Fewer denials due to accurate and complete submissions.
- Increased patient satisfaction and smoother workflows for staff.
By outsourcing their prior authorization management, the clinic regained valuable time and resources.
Key Takeaways
- Prior authorization is a vital part of the healthcare process for Medicare Advantage patients.
- While it ensures cost-effective and necessary care, it can also create delays and administrative challenges.
- Outsourcing to Staffingly, Inc. simplifies the process, reduces errors, and saves valuable time.
Conclusion
Prior authorization doesn’t have to be a roadblock. By partnering with a reliable outsourcing provider like Staffingly, Inc., you can streamline the process, improve efficiency, and deliver better patient care. Contact dan@staffingly.com or call (800) 489-5877 to learn how we can support your practice.
FAQs
1. Do all Medicare Advantage plans require prior authorization?
Not every service requires prior authorization, but high-cost or specialized procedures often do.
2. Can delays in prior authorization impact patient care?
Yes, delays can postpone essential treatments. That’s why efficient management is critical.
3. How can Staffingly improve the prior authorization process?
Staffingly handles the entire process, from documentation to appeals, ensuring faster approvals and fewer errors.
4. Is outsourcing prior authorization HIPAA-compliant?
Yes, Staffingly adheres to strict HIPAA guidelines to protect patient information.
5. How much can outsourcing prior authorization save my practice?
Outsourcing can save up to 70% on administrative costs, freeing your staff to focus on patients.
Disclaimer
The information in our posts informs and educates healthcare providers and readers seeking a better understanding of healthcare processes. It is not a substitute for professional advice.
Insurance requirements, policies, and approval processes can vary widely and change over time. Healthcare providers consult insurers or use professional resources for guidance. Patients reach out to insurance providers or healthcare professionals for specific advice.
This content does not establish any patient-caregiver or client-service relationship. Staffingly, Inc. assumes no liability for actions taken based on information provided in these posts.
For tailored support and professional services,
please contact Staffingly, Inc. at (800) 489-5877
Email : support@staffingly.com.
About the Author : Monica Michael is a seasoned Prior Authorization Specialist with years of experience in smooth insurance processes for healthcare providers. She is passionate about simplifying complex administrative tasks to help hospitals focus on delivering exceptional patient care.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



