On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
How Can Clinics Overcome Eligibility Verification Challenges in Mental Health Billing?
A mental health practice manager recently shared their frustration:
“Our EHR gives us ‘limited’ or ‘no information provided.’ No deductibles, no co-pays, nothing accurate. Patients expect answers, and we’re guessing.”
This isn’t an isolated story — it’s the daily reality for mental health clinics across the country.
From Availity’s inaccurate reports to EHRs like SimplePractice failing to deliver complete coverage data, behavioral health teams are spending hours on hold with payers, trying to confirm basic information that should take minutes.
Healthcare professionals in multiple forum discussions agree: eligibility verification has become one of the most broken processes in outpatient mental health.
Inaccuracies With Availity and Payers
Billing professionals across Reddit threads echoed the same problem: payer tools are unreliable.
“Availity marks every session as needing prior authorization — even when the plan clearly says no.”
“For BCBSIL, it shows ‘network not applicable’ even when we’re in-network. Then claims get denied as duplicates. I even had one denied because the system confused a patient with their twin.”
This confusion forces staff to spend hours confirming coverage for services they’ve already rendered.
Worse, payers’ own representatives sometimes provide incorrect information.
“They told us family therapy wasn’t covered. Turns out, they just didn’t understand the CPT code.”
These errors erode patient trust and make accurate cost estimates nearly impossible.
EHR System Limitations Create More Work
Clinics using SimplePractice reported that its “coverage reports” don’t show deductibles, co-pays, or co-insurance.
“We called support — they said the feature isn’t designed to give full results. What’s the point then?”
Some considered switching to AdvancedMD or eClinicalWorks, but those systems often need custom setup and training just to display accurate eligibility data.
This lack of visibility leaves clinics juggling multiple logins — EHRs, payer portals, and clearinghouses — just to get one patient’s information right.
A billing coordinator summarized it bluntly:
“We spend more time verifying benefits than seeing patients.”
Workflow Chaos and Burnout
Eligibility verification isn’t just frustrating — it’s a major driver of burnout in behavioral health administration.
“We handle nine providers’ authorizations. Half of the data comes back incomplete. Every denial ends up back on our desk.”
“It’s defeating. You start each day already behind.”
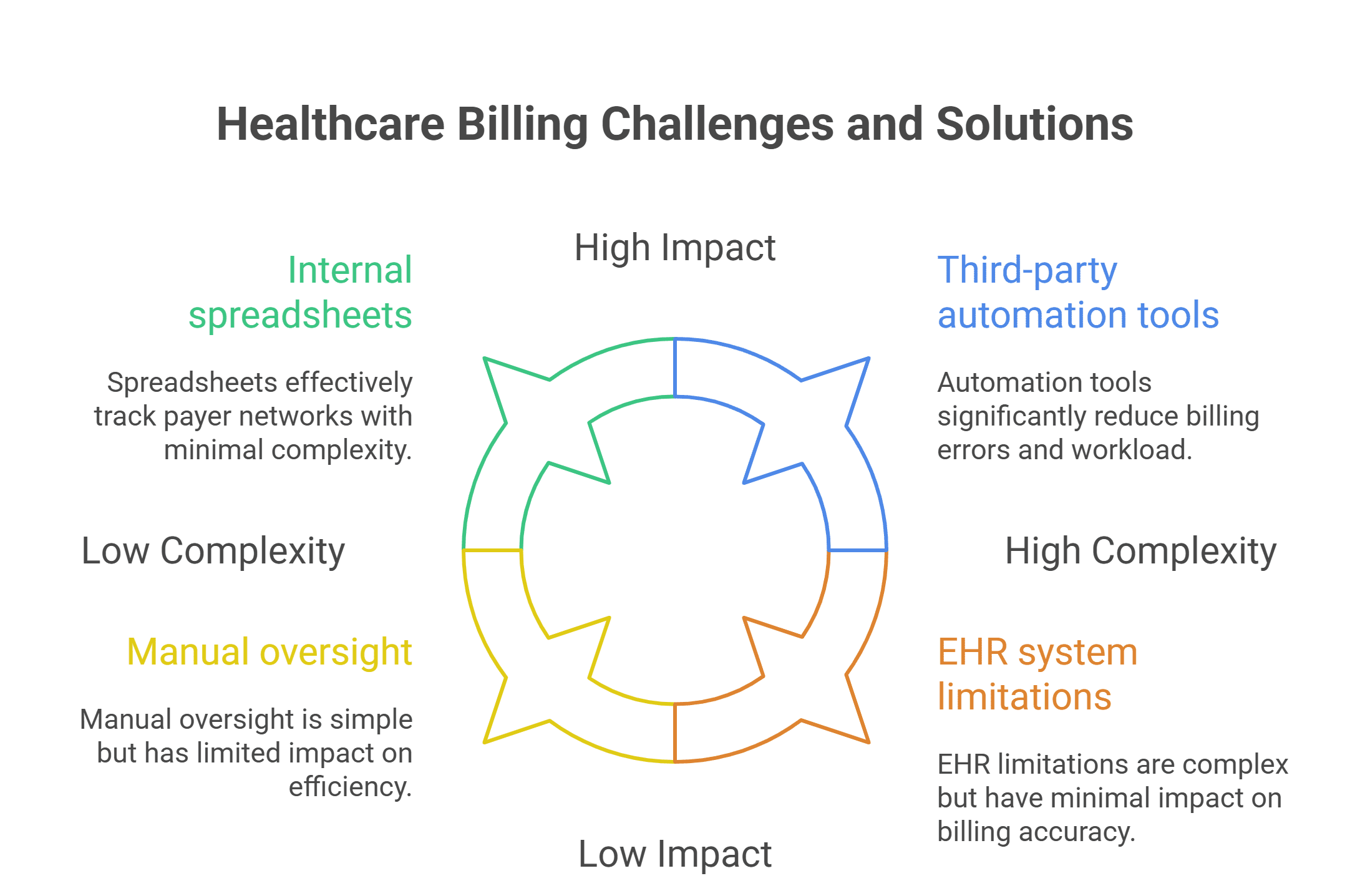
Because payer rules for behavioral health vary by therapy type, telehealth, and CPT code, automation tools often fail to interpret the nuances. Staff end up manually calling payers just to confirm coverage, creating long hours and endless spreadsheets.
As one user put it:
“It’s not just a payer problem. It’s a workflow problem.”
Provider Accountability and Communication Gaps
The issue doesn’t stop at technology — it’s also about provider responsibility.
“Providers prescribe sessions or therapies without checking if the plan covers them. Then we get blamed for denials.”
Clinics that implemented internal verification checklists saw improved results.
One mental health office shared:
“We built a form requiring diagnosis codes, CPT validation, and payer confirmation before scheduling therapy sessions. Our denials dropped by 40%.”
Shared accountability between providers and admin staff prevents chaos — and reduces patient confusion.
AI and Automation Are Helping — But Need Human Oversight
Many clinics have started experimenting with AI-powered verification tools that can automatically check payer portals, confirm benefits, and pre-fill eligibility forms.
But as one billing lead explained:
“AI tools can process data, but they can’t understand payers’ inconsistencies. You still need someone to interpret the results.”
That’s where hybrid AI + human systems are changing the game.
AI handles:
-
Payer portal lookups and data extraction
-
Benefit verification and documentation
-
Real-time updates to EMR systems
Human specialists handle:
-
Reviewing flagged results
-
Contacting payers for exceptions
-
Communicating coverage details to patients
This AI + Human Strategy reduces manual errors while ensuring every case is verified accurately.
How Staffingly Solves the Verification Bottleneck ?
Staffingly’s Virtual Eligibility Verification Specialists combine automation with clinical judgment to manage the entire process from start to finish.
✅ Eligibility & Benefits Verification: Real-time payer checks, including deductibles, co-pays, and co-insurance.
✅ AI-Augmented Verification Tools: Automated data collection across payer portals.
✅ Human Oversight: Healthcare-trained specialists validate and interpret payer results.
✅ Prior Authorization Support: Seamless handoff to authorization teams when required.
Each Staffingly specialist works remotely from India, Pakistan, or the Philippines, regions with strong healthcare education infrastructure. Many hold MD, RN, or PharmD degrees, bringing both clinical and operational expertise.
Compliance, Security, and Cost Advantage
Staffingly’s operations adhere to strict global compliance standards:
-
HIPAA-compliant for patient data protection
-
SOC 2 certified for secure operations
-
ISO 27001 certified for information security
Cost advantage:
-
U.S. in-house staff: $4,500–$6,000/month
-
Staffingly specialists: $9.50/hour, under $2,000/month full-time
That’s a 70% cost reduction — without sacrificing accuracy or compliance.
“Since outsourcing eligibility verification, our error rate dropped by 50% and we stopped losing patients over billing confusion,” one clinic reported.
AI + Human Model: Efficiency With Accountability
Smart practices are embracing hybrid operations — where AI reduces repetitive work, and human specialists ensure clinical accuracy.
This dual model ensures that every eligibility report is:
-
Verified in real-time
-
Cross-checked for payer-specific exceptions
-
Fully documented before patient visits
By combining automation and human insight, clinics are finally getting accurate data before the appointment, not weeks after.
Stop Losing Time on Incomplete Eligibility Checks
Eligibility Verification Shouldn’t Be Guesswork
If your staff is spending hours on hold, chasing payers, or explaining surprise bills — it’s time to fix your workflow.
15-Day Risk-Free Eligibility Verification Trial
✓ Virtual Eligibility Specialists – Verify benefits, deductibles, and co-pays accurately
✓ AI-Integrated Verification Tools – Speed up portal checks and reports
✓ HIPAA-Compliant, Healthcare-Trained Staff – Backed by MDs, RNs, and PharmDs
Starting at $9.50/hour — under $2,000 monthly vs $6,000+ local hires.
What Did We Learn?
-
Eligibility verification remains one of the biggest workflow challenges in mental health.
-
EHRs like SimplePractice often fail to provide accurate benefit details.
-
Availity and payer portals frequently show incomplete or incorrect data.
-
Manual calls create burnout and billing confusion.
-
Hybrid AI + human verification models dramatically improve accuracy and speed.
-
Outsourcing to compliant, trained virtual specialists cuts costs by 70%.
What People Are Asking?
Q1. Why is eligibility verification so unreliable?
Because payer portals and EHRs often provide incomplete or outdated benefit data.
Q2. Can automation fix this problem?
Partially — AI speeds up lookups, but human oversight ensures accuracy.
Q3. Which EHRs handle eligibility best?
AdvancedMD and eClinicalWorks offer detailed reports but require setup and training.
Q4. How can clinics reduce denials?
By verifying benefits pre-visit, documenting payer confirmation, and using hybrid verification teams.
Q5. What’s the cost advantage of outsourcing eligibility work?
Up to 70% savings — under $2,000/month compared to $6,000+ for local staff.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services
Please contact Staffingly, Inc. at (800) 489-5877
Email: support@staffingly.com
About This Blog: This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



