On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesPHARMACIST CLINICAL REVIEW PROCESS

Author: M. KAVYA (IV/VI PHARM D)
Chebrolu Hanumaiah institute of pharmaceutical sciences, Chowdavaram, Guntur
ABSTRACT:
Prescription of medicines is a fundamental component of the care of older people, but evidence suggests that pharmacotherapy in this population is often not suitable. Pharmacists have been involved in different methods for the optimization of prescribing and rational medication use in older people. This article tells about the different models of care in which pharmacists are involved in the optimization of pharmacotherapy in older people, and reviews the impact of these approaches on both process and outcome measures. The provision of pharmaceutical care, medication reviews and educational interventions by pharmacists in the nursing home, ambulatory and acute care settings are discussed. From the literature reviewed, it is clear that when pharmacists play a proactive role in performing medication reviews. However, the evidence of the impact of pharmacists’ interventions on health outcomes, quality of life or cost-effectiveness of care is mixed. Better results have been reported in the context of a multidisciplinary team. Opportunities remain for multicentre, European-based, pharmacist-intervention trials in all settings, to determine the effectiveness and economic benefit of pharmacist involvement in the optimization of pharmacotherapy in older people.
INTRODUCTION:
The prescription of medicines is an important component of the care for older people, but evidence suggests that the use of medicines in this population is often not suitable for many multiple reasons, such as complexities of prescribing the patient and health system factors. This in turn can have serious effects such as adverse drug events (ADEs) and an also increase in the utilization of healthcare services, and costs. According to published studies, 10–30% of hospital admissions in older people are directly related to drug-related problems (DRPs),[3-5] and ADEs are documented in 5–35% of older patients in the community that may lead to hospital admissions in 6–16% of cases. They include educational approaches, medication reviews, computerized systems, geriatric evaluation and management teams, and pharmacist interventions. The terms that are most commonly used to describe pharmacists’ involvement in patient care are ‘clinical pharmacy’ or ‘pharmaceutical care’. The aim of pharmaceutical care is based on a process by which a pharmacist interact with a patient and/or other healthcare professional (HCP) to reduce pharmacotherapy, by designing, implementing and monitoring therapeutic goals that will give specific therapeutic outcomes for patients.
Role and Impact of the Pharmacist in the Nursing Home Setting:
Several recent systematic reviews of pharmacists’ interventions in nursing home patients remarked on the varied roles of the pharmacist within the long-term care/nursing home setting, such as
- Performing regular medication reviews.
- Being an active member of a multidisciplinary team.
- Enhancing the knowledge of physicians, nurses and patients with regard to safer medication usage.
Medication reviews performed by pharmacist:
The reviews that was carried out by the pharmacists resulted in many more changes per patient medication regimen than those performed by GPs; however, the changes that were actually accepted by the patient’s physicians (77%) was not result any one in statistically significant reductions in either drug costs or rate of hospitalizations. A more recent observational study done in the Netherlands demonstrated statistically significant decrease in DRPs following the implementation of pharmacist-led reviews in 30 patients. Studies have also reported on the role of a pharmacist as part of a larger multidisciplinary team conducting medication reviews. Schmidt et al.[38] reported on the findings on pharmacists’ interventions in 33 nursing homes in Sweden. The study involved doctors, pharmacists, nurses and nursing assistants working together as part of a multidisciplinary team. The intervention main motto to reduce the rate of inappropriate prescribing of psychoactive medications such as antipsychotics, hypnotics and anxiolytics. The intervention has conducted case conferences discussing the prescribing of such medications. The results from the homes that were randomized to the intervention showed that the mean numbers of psychoactive medications and therapeutic duplications do not change over time, although there was a reduction in the prescribing of antipsychotics, hypnotics and antidepressants. During the same period, the prescribing of psychoactive medications and therapeutic duplications increased in the nursing homes to normal care. The authors decided that the multidisciplinary nature of the intervention was key to the success of this intervention.[38,39] More recently, Halvorsen et al.[40] published the findings of a multidisciplinary intervention with regard to resolving DRPs in Norwegian nursing homes.
Role and Impact of the Pharmacist in the Ambulatory Care Setting:
In reducing the pharmacotherapy of older people in the ambulatory setting, based on published RCTs. Both reviews had evidence that medication management services and pharmaceutical care services reduce the several countries, pharmaceutical care provided to community-residing patients has been specifically encouraged, e.g. in the US, UK, Canada, Netherlands, Australia and New Zealand. In the UK, for example, the National Service Framework for older people had medication reviews to decease the medicine-related problems faced by older people.[49,50] This uses the development of research projects that aimed to evaluate the impact of these medication reviews. Several of these studies have been published. Two subsequent reviews done by Hanlon and colleagues[2,6] have already talked the role of pharmacists occurrence of DRPs. Unfortunately, the evidence was the effect of such services on clinical outcomes, health-related quality of life and effectiveness was found to be limited.
Interventions by Community Pharmacists in the Community Pharmacy Setting:
Several huge intervention studies conducted in Europe evaluated the effect of structured pharmaceutical care provided by community pharmacists to older outpatients. In the PEER study (Pharmaceutical care of the Elderly in Europe Research), Bernsten et al.[12] the outcomes of a structured pharmaceutical care programme given by community pharmacists to older patients taking at least four medications. The trial involved 104 intervention and 86 control pharmacy sites, and 1290 intervention and 1164 control patients from seven European countries. No differences in primary outcomes (health-related quality of life, hospitalizations and associated costs) were found. There were some positive, but result was not statistically significant, changes in certain process measures in patients in the intervention group. Some health improvements were observed in the intervention Pharmacist Role in Pharmacotherapy for Older People 503 Adis ª 2012 Springer International Publishing AG.
The RESPECT trial (Randomised Evaluation of Shared Prescribing for Elderly people in the Community over Time) was another larger trial aimed at deceasing the effectiveness and cost effectiveness of pharmaceutical care provided by 62 community pharmacists to 760 older people in the UK.[15,16] The results of the RESPECT trial have showed the findings of the PEER study. The intervention had lead to significant changes in the appropriateness of prescribing or quality of life. The researchers identified that it was often challenging to fully implement pharmaceutical care in the community because in the difficulties in collecting and accessing patient data, and to use organize meetings to discuss care plans with GPs. the training was limited to two sessions. Analyses of cost effectiveness had led to uncertain results. In the cohort of older patients involving in the study, pharmaceutical care services had estimated to be cost effective mainly in younger subjects with fewer medications.
Role and Impact of the Pharmacist in the Acute Care Setting:
The role of clinical pharmacists in acute care has over time, with increased basis on collaborative care and patient involvement.[56] An review found that interacting with the healthcare team on patient rounds, counceling patients, reconciling medications, and providing patient discharge and follow-up all had involved in improved outcomes such as ADEs, medication errors, medication knowledge and length of stay.[56] Different surveys have been conducted to describe the level of implementation of clinical services by pharmacists in the acute care setting.
Among European pharmacists that were assigned one or several clinical specialties, 7% worked in geriatric units, which was large behind the percentage of pharmacists working in critical care (35% of respondents) or in surgery (20% of respondents). The results must be interpreted with caution given the relatively small number of respondents.
Spinewine et al.[21] performed an RCT to evaluate the use of the pharmaceutical care provided in addition to acute geriatric evaluation and management care on the use of prescribing. 203 patients admitted to an acute geriatric unit in Belgium were randomized. When comparing appropriateness of prescribing on admission and at discharge, intervention patients are have more likely than control patients to have an improvement in the Medication Appropriateness Index (MAI) and in seven criteria of underprescribing. With regard to clinicaloutcomes, the authors reported an toward decreased rates of mortality and emergency department visits, but the study was not much to detect significant differences Overall, 90% of the interventions that made by the clinical pharmacist were improved.
Role and Impact of the Pharmacist on Continuity of Care:
In addition to the above studies, many studies specifically evaluated the impact of interventions provided by pharmacists at the moment of transition across settings of care. Most studies on the transition from hospital to the community or the nursing home setting. Two RCTs were performed in the UK. Nazareth et al.[25] found no effect with use to the implementation of a pharmaceutical discharge plan plus home visits after discharge on hospital readmission, medication knowledge and adherence, and patient satisfaction. In contrast, Al Rashed et al.[26] reported that inpatient pharmaceutical counselling, linked to a medication and information discharge summary any and a medicine reminder card, attributed to better drug knowledge and compliance together with decrased unplanned visits to the doctor and readmissions. A pharmaceutical managment visit consolidated the decreased healthcare outcomes. A recent review on the effect of interventions to minimise drug-related problems in older people after discharge concluded that the interventions tested have not given appropriate results.
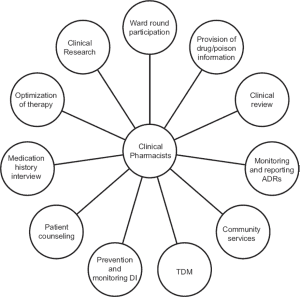
FLOW CHART FOR REVIEW PROCESS:
Patient Registration
Patients problems concerns
- Based on medication use
- Based on patient concern
- Based on physical complaint
- And others
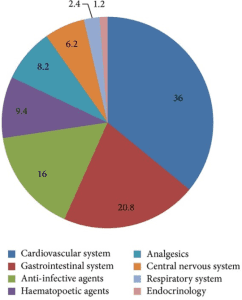
THE PIE CHART SHOWING VARIOUS CLASSES OF DRUGS PRESCRIBED FOR PATIENTS TO GENERATE DATA ON DRUG UTILISATION PATTERN AND COST OF DRUG TREATMENT.
CONCLUSION:
This review has updated previously published by including several recent European studies. From the literature reviewed, it is clear that when pharmacists play a important role in performing medication reviews and in the active education of other HCPs, pharmacotherapy for older patients is improved. However, the evidence of the impact of pharmacists’ interventions on health outcomes, quality of life or cost effectiveness of care is mixed. One reason might be that the wrong health outcomes have been used. In fact, mortality, utilization of heathcare services and quality of life are all multifactorial. Further research should focus on outcomes that are more responsive to pharmacy interventions, such as ADEs. It is apparent from the studies reviewed that in order for pharmacists to add significant value to the optimization of older patients’ pharmacotherapy, they need to combine closely with other HCPs (mainly physicians and nurses). Better outcomes have been documented when the pharmacists have had access to patient records, and have actively spoken with patients and other HCPs as part of a multidisciplinary team. Further in-depth analysis is warranted to identify additional factors that are fundamental to success.
REFERENCES:
- Spinewine A, Schmader KE, Barber N, et al. Appropriate prescribing in elderly people: how well can it be measured and optimised? Lancet 2007 Jul; 370 (9582): 173-8
- Hanlon JT, Lindblad CI, Gray SL. Can clinical pharmacy services have a positive impact on drug-related problems and health outcomes in community-based older adults? Am J GeriatrPharmacother 2004 Mar; 2 (1): 3-13
- Kongkaew C, Noyce PR, Ashcroft DM. Hospital admissions associated with adverse drug reactions: a systematic review of prospective observational studies. Ann Pharmacother 2008 jul(42) 7.
- Zermansky AG, Alldred DP, Petty DR, et al. Clinical medication review by a pharmacist of elderly people living in care homes: randomised controlled trial. Age Ageing 2006 Nov; 35 (6): 586-9
- Patterson SM, Hughes CM, Crealey G, et al. An evaluation of an adapted US model of pharmaceutical care to improve psychoactive prescribing for nursing home residents in Northern Ireland (Fleetwood Northern Ireland study). J Am GeriatrSoc 2010 Jan; 58 (1): 44-5
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



