On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
How Proactive Insurance Verification Transforms Your Workflow?
When we talk about improving patient intake, everyone jumps to “wait times” or “online scheduling.” But there’s one quiet process that can make or break the whole experience: insurance verification.
It’s not flashy. It’s not something patients ever thank you for. But get it wrong, and everything else unravels: delays, denials, patient frustration, and serious billing headaches.
“You can give a patient world-class care—but if the insurance isn’t right, they remember that instead.”Insurance verification isn’t just paperwork. It’s the foundation of every successful visit.

Key Takeaways
-
Insurance verification isn’t just admin work—it’s the backbone of every patient visit.
When it’s missed or rushed, it causes billing delays, denials, and patient frustration. -
Most front desk teams are stretched too thin to verify every detail accurately.
They’re juggling phones, check-ins, scheduling, and insurance—all at once. -
Poor insurance checks lead directly to revenue loss.
Denied claims, rework, and patient dissatisfaction cost far more than clinics realize. -
Outsourcing insurance verification takes pressure off staff and boosts accuracy.
Trained, HIPAA-compliant support teams can verify coverage in advance—fast and reliably. -
Proactive verification improves the patient experience.
When coverage is confirmed before the visit, there are fewer surprises and smoother check-ins. -
Automation + expert support = the sweet spot.
Use tech to handle repetitive steps, and pair it with people who know the ins and outs of payer systems. -
Solving this one piece of your workflow can unlock better care, better revenue, and less burnout.
It’s a simple fix with a big impact.
| Verification Gap | Operational Impact | Financial Impact | Patient Experience |
|---|---|---|---|
| Incomplete eligibility checks | Claim rework & delays | Denied reimbursement | Billing confusion |
| Same-day verification | Front desk overload | Delayed collections | Long check-in times |
| Outdated insurance data | Billing corrections | Lost revenue | Surprise bills |
| Manual verification workflows | Staff burnout | Higher admin costs | Lower trust |
| Missed plan limitations | Denied procedures | Write-offs | Canceled visits |
The Reality of Insurance Verification Bottlenecks
Let’s be real: insurance eligibility checks are often messy, manual, and frustrating.
Every day, front office staff are stuck:
-
Calling insurance companies and sitting on hold.
-
Logging into clunky portals that time out.
-
Double-checking copays, deductibles, and plan changes.
-
Dealing with outdated or incorrect patient information.
And they’re doing all this while juggling phones, appointments, and walk-ins.
“Half my day is spent trying to get someone on the phone at the insurance company. The other half is cleaning up the mess from when we couldn’t.”
It’s no wonder mistakes happen—and they cost more than people realize.

The Patient Impact No One Talks About
Insurance hiccups don’t just frustrate staff—they directly affect patients:
-
They show up thinking they’re covered… and find out they’re not.
-
Copays surprise them. Deductibles confuse them.
-
Their procedures get postponed.
-
Their claims get denied.
“The patient’s upset—but we’re the ones who tried three times to confirm coverage. The system failed us both.”
This damages patient trust, slows down care, and leads to lost revenue when patients walk away.
Why Clinics Struggle With Eligibility Checks
Here’s the truth: most clinics just don’t have time to verify every detail before a visit.
Why?
-
It’s time-consuming. Some plans require 15+ minutes to verify. Multiply that by a full day’s schedule.
-
It’s complicated. Plans, deductibles, coverage types—it’s a moving target.
-
It’s reactive. Most clinics check eligibility the day of (or worse, during check-in).
“We’re trying to verify coverage with five people in the lobby and phones ringing nonstop.”
And when eligibility checks get rushed or skipped, everyone pays for it later.
The Revenue Cost of Incomplete Verification
Here’s what happens when verification isn’t done—or isn’t done well:
-
Claim denials. One missing piece of info can void reimbursement.
-
Delayed billing. Staff spend days chasing down eligibility after the fact.
-
Frustrated patients. No one likes surprise bills or canceled procedures.
-
Lost revenue. Denied or delayed claims = money left on the table.
“We lost over $12,000 in one quarter just from claims denied over insurance verification issues.”
Smarter Solutions to Fix the Verification Gap
The good news? You don’t have to overhaul your whole system—just improve how you handle this one piece.
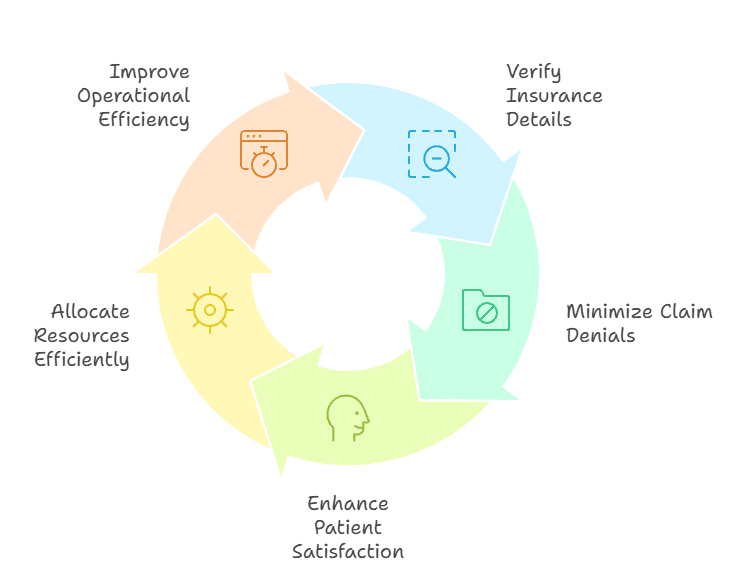
1. Outsource Insurance Verification to Experts
Let trained, HIPAA-compliant virtual teams handle the insurance calls, portal logins, and data entry—before the patient arrives.
“Once we outsourced insurance checks, the denials dropped almost overnight.”
2. Move From Reactive to Proactive
Get insurance verified days before the appointment, not during check-in. That way, there’s time to clarify coverage or prep the patient.
“We send eligibility checks 48 hours before visits. No more surprises.”
3. Use Smart Tools + People
EMR-integrated platforms + outsourced staff = fast, accurate, and reliable verifications—without burdening your front desk.
“Our front office doesn’t touch insurance anymore. It’s all done behind the scenes.”
What Did We Learn?
Insurance verification may seem like a small step, but it affects everything in your practice.
Here’s what we covered:
-
It’s a major source of errors and denials—but often overlooked.
-
Patients feel the pain when it’s done poorly.
-
In-house staff rarely have the time or tools to do it consistently.
-
Outsourcing and automation make the process smoother, faster, and far more accurate.
What People Are Asking?
Q: What’s the most common mistake in insurance verification?
A: Rushing through it—or skipping it entirely. That leads to claim denials and surprise bills.
Q: How does poor verification affect cash flow?
A: Denied claims delay or eliminate revenue. Each one adds cost and stress to your billing team.
Q: Can outsourcing insurance verification really save money?
A: Absolutely. You reduce denial rates, increase collections, and free up your front office staff to focus on patients.
Q: Isn’t insurance info already in the EMR?
A: Yes, but it’s often outdated. Plans change. Deductibles reset. Real-time verification is the only way to be sure.
Q: How fast can outsourcing services verify eligibility?
A: Many outsourced teams confirm coverage within 24 hours—well before the patient even arrives.
A Smarter Way Forward
Insurance verification may not be glamorous, but it’s critical. And when it’s done right—accurately, ahead of time, and with expert help—everything else runs smoother.
Fewer denials. Happier patients. Better revenue.
Staffingly, Inc. offers Insurance Eligibility Verification services that take this burden off your team and protect your bottom line.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services
Please contact Staffingly, Inc. at (866) 938-1894
Email: support@staffingly.com
About This Blog: This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



