On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
Why Proactive Compliance with Virtual Billing Assistants Ensures Audit Success?
When Dr. Ramirez received an audit letter from Medicare, his stomach dropped. He hadn’t done anything wrong—at least, he didn’t think so. His team worked hard, saw patients, submitted claims. But the audit flagged $58,000 in services. Suddenly, the clinic wasn’t just healing patients—it was fighting for its financial life.
Compliance in medical billing isn’t just paperwork. It’s protection. It’s reputation. And it’s the difference between smooth operations and a costly shutdown.
Why This Matters Today?
Audits are no longer rare—they’re expected. From Medicare to commercial insurers, payers are ramping up their review processes to reduce fraud, waste, and abuse. But too often, providers are unprepared until it’s too late.
-
Penalties can reach six figures—even for honest mistakes
-
Failed audits may trigger reputational damage or exclusion from payer networks
-
Lack of training and poor documentation are the top culprits
The good news? With the right systems, teams can transform compliance into a strategic strength, not just a legal obligation.
Key Insights: Types of Audits and What Triggers Them
Common Types of Audits
-
Government Payers (Medicare/Medicaid)
-
Recovery Audit Contractors (RACs) review overpayments and underpayments
-
Office of Inspector General (OIG) investigates fraud and abuse
-
Medicaid audits are state-run but follow similar protocols
-
-
Commercial Insurance Audits
-
Focused on coding accuracy, medical necessity, and contractual compliance
-
-
Targeted Probe & Educate (TPE)
-
CMS initiative to identify high-error providers and offer education + re-review
-
-
Internal Audits
-
Proactive, internal reviews to spot issues before payers do
-
Audit Triggers
-
Unusually high coding levels (e.g., always billing 99215)
-
High denial or appeal rates
-
Whistleblower complaints
-
Patient-reported billing discrepancies
-
Failure to adapt to policy changes
-
Red flags from payer analytics and algorithms
Building a Culture of Compliance
1. Clear Policies
-
Commitment to correct coding and billing
-
Ban on upcoding/unbundling
-
HIPAA and data security adherence
-
Medical necessity rules
-
Procedures for reporting suspected fraud
2. Strong Procedures
-
Step-by-step guides for charge entry, claim submission, denial management
-
Clearly defined workflows for record-keeping and appeals
-
Regular process updates tied to changing payer policies
3. Ongoing Staff Training
-
Comprehensive onboarding for coders, front desk, and clinicians
-
Annual or semi-annual refresher courses
-
Documented attendance, assessments, and curriculum
-
Safe channels for questions or reporting concerns
A well-trained team is your first line of defense against audit risk.
Documentation: The Cornerstone of Defense
In healthcare billing, if it isn’t documented—it didn’t happen.
Auditors want proof, not assumptions. That means clear, complete, and timely records that directly support each billed service.
Documentation Must-Haves
-
Justify medical necessity (symptoms, diagnosis, treatment plan, response)
-
Avoid generic templates—make notes patient-specific
-
Capture all elements of E/M visits: history, exam, decision-making
-
Provider signatures, dates, and credentials on every entry
-
Modifier use must be explained in the chart
-
Diagnosis and procedure codes must logically align
Regular internal chart audits are a smart way to stay ahead of payer reviews.
Coding Accuracy: The Language of Reimbursement
Every code is a financial signal. Misuse can result in denials, clawbacks, or worse—fraud accusations.
Foundations of Accurate Coding
-
Codes must be supported by documentation
-
Follow LCDs/NCDs and payer-specific rules
-
Use up-to-date CPT, ICD-10, and HCPCS manuals
-
Know when and how to apply modifiers (-25, -59, etc.)
-
Avoid overcoding (billing higher levels than documented)
-
Watch for bundling edits and NCCI compliance
Hiring certified coders and maintaining regular coding audits is essential.
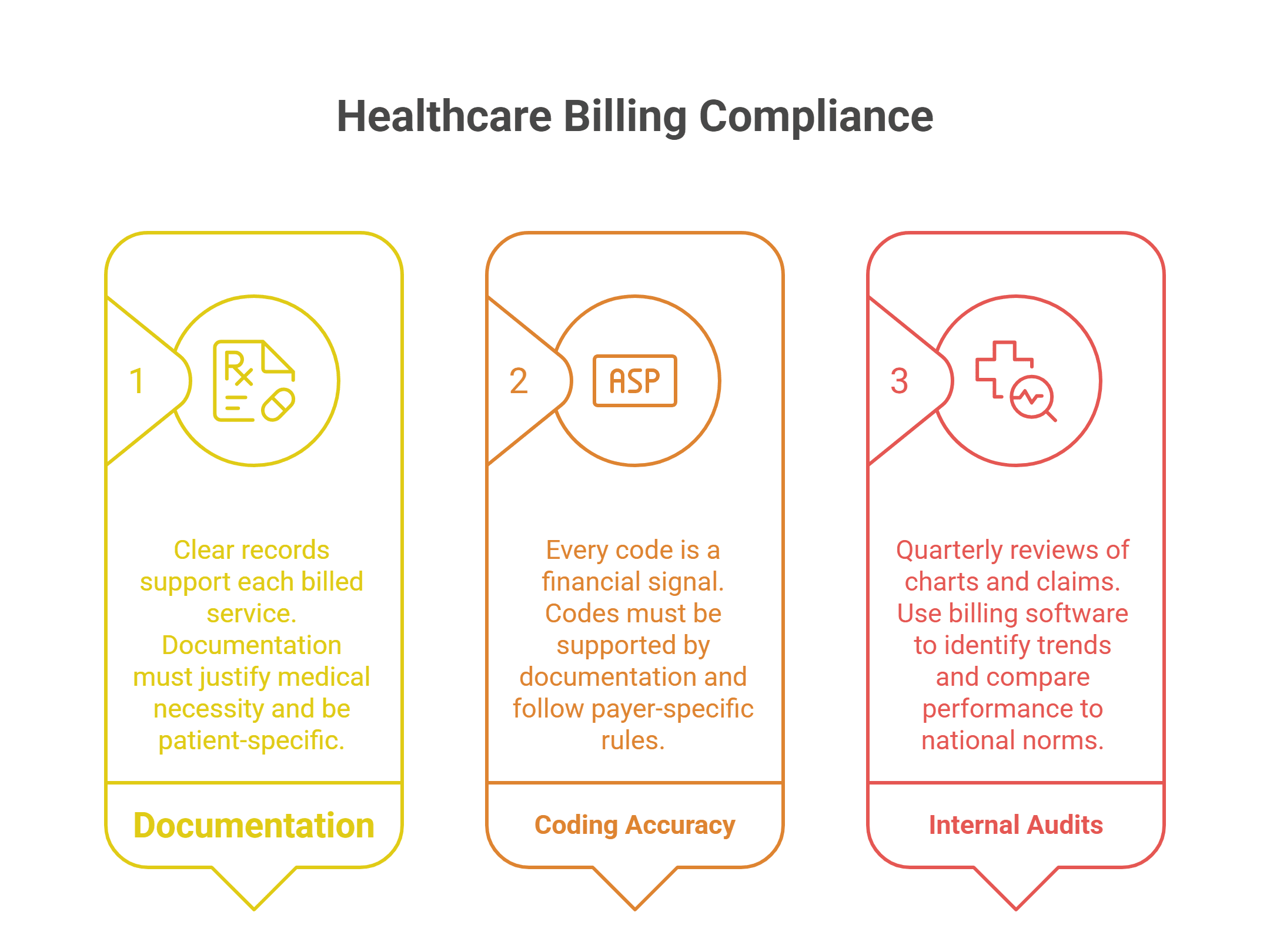
Internal Audits & Monitoring: Your Compliance Radar
Being audit-ready means thinking like an auditor—before they arrive.
How to Monitor Proactively?
-
Internal Audits: Quarterly reviews of random charts and claims
-
Data Analytics: Use billing software to identify trends like:
-
Frequent denials
-
Modifier misuse
-
E/M level outliers
-
Payer-specific rejection patterns
-
-
Benchmarking: Compare your performance to national coding norms
Catch and correct problems internally to avoid surprises from external audits.
How to Respond to an Audit (Without Panic)?
Audit letter just landed? Don’t panic—plan.
-
Verify Scope and Source: Who is auditing? What’s being requested?
-
Assign a Point Person: Centralize communications
-
Stick to What’s Requested: Don’t overshare
-
Don’t Alter Records: Never modify documentation after the fact
-
Seek Legal or Compliance Help: Especially for high-stakes audits
-
Appeal Smartly: Build your case with documentation, payer policies, and timelines in mind
Every step should reflect calm, clarity, and control.
Staffingly’s Role in Compliance Support
At Staffingly, we don’t just place virtual medical assistants—we train billing and coding professionals who understand compliance from day one.
Our assistants:
-
Follow HIPAA and payer-specific policies
-
Support pre-claim scrubbing, coding accuracy, and documentation audits
-
Are trained on eClinicalWorks, AdvancedMD, Kareo, Athena, and more
-
Provide real-time support for denials, modifiers, and appeals
We help practices build audit-ready workflows—without burning out in-house teams.
What Did We Learn?
-
Compliance isn’t optional—it’s strategic. Practices that build proactive systems are better protected from audits, penalties, and revenue loss.
-
Most audits are triggered—not random. High denial rates, unusual billing patterns, or outdated coding can set off red flags.
-
Clear documentation and accurate coding are non-negotiable. They’re your first line of defense.
-
Internal audits and monitoring matter. Waiting for external payers to flag issues puts your practice at risk.
-
Trained support staff make a difference. Virtual billing assistants—like those provided by Staffingly—play a vital role in enforcing compliance without overloading in-house teams.
What People Are Asking
1. What types of audits should healthcare providers expect?
Government (Medicare/Medicaid), commercial insurers, CMS TPE reviews, and internal audits are all common.
2. What triggers a medical billing audit?
Frequent high-level coding, repeated denials, patient complaints, whistleblower reports, or failure to follow policy updates.
3. How can practices prepare for audits in advance?
With written compliance policies, training, accurate documentation, routine internal audits, and proactive data monitoring.
4. What’s the role of virtual billing assistants in compliance?
They help ensure accurate claims, perform pre-submission checks, flag issues early, and maintain payer-specific billing standards—all remotely and securely.
5. What happens if we fail an audit?
Practices may face repayment demands, fines, reputational damage, and in serious cases, exclusion from payer networks.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services,
Please contact Staffingly, Inc. at (800) 489-5877
Email : support@staffingly.com.
About This Blog : This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



