On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
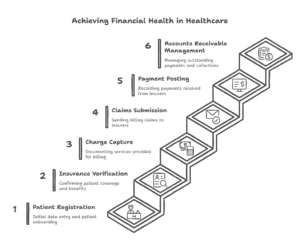
Revenue Cycle Management Steps

Revenue Cycle Management (RCM) is the financial backbone of any healthcare organization. It ensures that medical services are accurately documented, claims are submitted correctly, and payments are collected efficiently. Without a well-structured RCM process, healthcare providers risk delayed reimbursements, claim denials, and financial instability.
In this guide, we will break down all the revenue cycle management steps, from patient registration to payment posting. Whether you’re a small clinic or a large hospital, understanding and optimizing these steps can improve cash flow and reduce administrative burdens.
Understanding Revenue Cycle Management (RCM)
RCM is the process of managing financial transactions related to patient care, from the initial appointment to the final payment. It involves several steps, ensuring that healthcare providers receive timely and accurate reimbursement for the services they provide.
A well-managed RCM process:
- Reduces claim denials
- Improves revenue collection
- Enhances patient experience
- Ensures compliance with healthcare regulations
By following the revenue cycle management steps outlined below, healthcare organizations can streamline operations and maintain financial stability.
Key Revenue Cycle Management Steps
1. Patient Registration
Patient registration is the first and most crucial step in the RCM process. It involves collecting accurate demographic and insurance information from new and returning patients.
What Happens During Patient Registration?
- Collect patient name, date of birth, address, and contact details
- Verify identity using government-issued IDs
- Obtain insurance details, including policy number and coverage information
- Check for outstanding balances or unpaid claims from previous visits
Why is Patient Registration Important?
Errors in patient registration can lead to claim denials and payment delays. Ensuring that all information is correct at this stage helps avoid administrative headaches later.
2. Insurance Verification
Before a patient receives medical services, their insurance coverage must be verified. This step ensures that the patient’s insurance plan covers the required services and determines the patient’s financial responsibility.
How Does Insurance Verification Work?
- Contact the insurance provider to confirm active coverage
- Verify copayments, deductibles, and out-of-pocket costs
- Identify any coverage limitations or prior authorization requirements
- Inform patients about their payment responsibilities
Benefits of Insurance Verification
By verifying insurance before the appointment, healthcare providers can prevent claim rejections and unexpected patient billing issues.
3. Charge Capture
Charge capture is the process of recording and documenting all medical services provided to a patient. Every service, procedure, or treatment must be accurately documented to ensure proper reimbursement.
Key Aspects of Charge Capture
- Physicians and nurses record services in the Electronic Health Record (EHR) system
- All procedures are assigned appropriate medical codes
- Charges are reviewed for accuracy before submission
Why is Charge Capture Critical?
Errors in charge capture can lead to lost revenue. If a service is not recorded correctly, the provider may not receive payment for it.
4. Medical Coding
Medical coding translates healthcare diagnoses, procedures, and services into standardized codes used for billing. These codes ensure that insurance companies understand what services were provided and how much they should reimburse.
Types of Medical Codes Used in RCM
- ICD-10 Codes: Used for diagnosing conditions
- CPT Codes: Used for documenting procedures and treatments
- HCPCS Codes: Used for additional services like durable medical equipment
Importance of Medical Coding
Accurate medical coding ensures proper claim reimbursement. Incorrect codes can lead to claim denials, audits, or compliance violations.
5. Claim Submission
Once medical services are coded and charges are documented, the next step is claim submission. Healthcare providers send claims to insurance companies, detailing the services provided and requesting payment.
Steps in Claim Submission
- Verify patient information and insurance details
- Ensure that all medical codes are accurate
- Submit claims electronically through billing software
- Monitor claim status and address any issues
Avoiding Claim Denials
Insurance companies reject claims for many reasons, including missing information, incorrect codes, or expired policies. Proper claim submission minimizes these risks.
6. Denial Management
Not all claims are approved on the first attempt. Some are denied due to errors, missing information, or coverage issues. Denial management focuses on identifying, analyzing, and resolving claim denials to recover lost revenue.
Denial Management Process
- Identify the reason for claim denial
- Correct errors and resubmit claims
- Appeal denied claims if necessary
- Track denial trends to prevent future issues
Why Denial Management Matters
Denied claims represent lost revenue. A strong denial management strategy ensures that providers collect the payments they are owed.
7. Payment Posting
Once an insurance company processes a claim, payments are sent to the healthcare provider. Payment posting involves recording these payments in the provider’s financial system.
Steps in Payment Posting
- Post payments received from insurance companies and patients
- Identify any discrepancies between billed and paid amounts
- Apply adjustments for contractual agreements or write-offs
- Reconcile payments with bank deposits
Impact of Payment Posting
Proper payment posting ensures that providers have a clear picture of their financial health. It also helps identify unpaid balances that require further follow-up.
8. Prior Authorization
Prior authorization is required for certain medical procedures, treatments, and medications. It ensures that insurance companies approve a service before it is provided, preventing claim denials later.
How Prior Authorization Works
- Submit a request to the insurance provider
- Provide medical documentation supporting the request
- Await approval before proceeding with the service
Why Prior Authorization is Essential
Without prior authorization, insurance companies may refuse to cover certain services, leading to financial loss for both the provider and patient.
9. Other Essential RCM Steps
Service Delivery
The actual medical service or treatment is provided to the patient, ensuring quality care and documentation for billing.
Claim Preparation
Before submitting claims, providers double-check documentation, ensuring accuracy and compliance with payer requirements.
Reporting and Analytics
Healthcare organizations track financial performance, identify trends, and make data-driven decisions to improve revenue cycle efficiency.
| RCM Step | Primary Purpose | Common Errors | Outsourcing Benefit |
|---|---|---|---|
| 1. Patient Registration | Collect demographic/insurance data | Incomplete patient info | Automated data validation |
| 2. Insurance Verification | Confirm coverage/copays | Expired policies | Real-time eligibility checks |
| 3. Charge Capture | Document all services | Missed billable services | EHR integration specialists |
| 4. Medical Coding | ICD-10/CPT/HCPCS coding | Incorrect code selection | Certified coders 98% accuracy |
| 5. Claim Submission | Electronic claim filing | Missing documentation | Pre-scrubbing 95% clean claims |
| 6. Denial Management | Appeal/resolve rejections | Late appeals | 70% denial recovery |
| 7. Payment Posting | Record EOB payments | Payment-application errors | Automated reconciliation |
| 8. Prior Authorization | Pre-service approvals | Missing PA requirements | 90% first-pass approval |
What Did We Learn?
Understanding the revenue cycle management steps is essential for healthcare providers aiming to optimize their financial operations. Key takeaways include:
- Accurate patient registration and insurance verification prevent billing errors
- Charge capture and coding ensure all services are documented correctly
- Claim submission and denial management maximize reimbursements
- Payment posting and prior authorization streamline cash flow and compliance
By refining each step of the revenue cycle, healthcare providers can reduce claim denials, improve cash flow, and focus on delivering quality care.
What People Are Asking?
1. What is revenue cycle management in healthcare?
Revenue Cycle Management (RCM) is the process of managing a patient’s financial transactions, from appointment scheduling to final payment collection.
2. Why is insurance verification important in RCM?
Insurance verification ensures that the patient’s coverage is active and determines their financial responsibility, reducing claim rejections.
3. How can providers reduce claim denials?
By ensuring accurate patient registration, proper coding, and timely submission of claims, providers can minimize denials.
4. What role does medical coding play in RCM?
Medical coding translates healthcare services into standardized codes, ensuring proper claim submission and reimbursement.
5. How can outsourcing RCM services benefit healthcare providers?
Outsourcing to companies like Staffingly, Inc. helps providers focus on patient care while experts handle billing, coding, and claim management.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services,
please contact Staffingly, Inc. at (800) 489-5877
Email : support@staffingly.com.
About This Blog : This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



