On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing ServicesSummarize this blog post with:
How to Handle Clinical Questions in Prior Authorization Requests in Atlanta

Prior authorization isn’t just paperwork—it’s a crucial step in ensuring that medical treatments are both necessary and covered by insurance. For healthcare providers in Atlanta, effectively handling clinical questions in prior authorization can be the key to securing swift approvals and avoiding costly delays. Answering these questions accurately isn’t just about meeting insurer requirements—it’s essential for maintaining a strong revenue cycle and providing quality patient care.
Understanding Clinical Questions in Prior Authorization
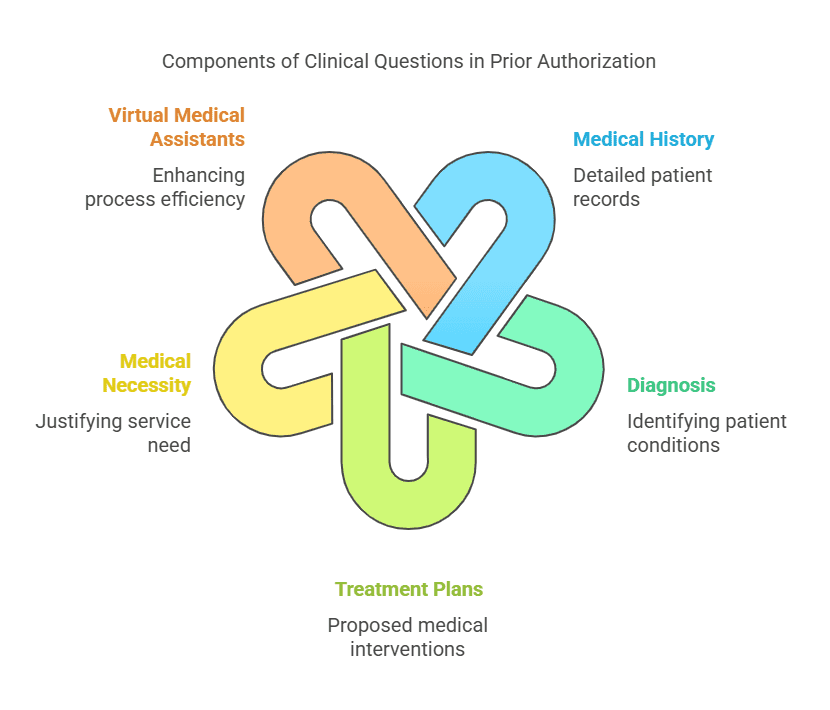
Clinical questions are often at the heart of prior authorization. They provide the rationale for treatments or procedures, fulfilling insurance requirements that ensure appropriate care.
What Are Clinical Questions in Prior Authorization?
Clinical questions ask for detailed information about a patient’s medical history, diagnosis, or treatment plans to justify the requested service. These queries link directly to medical necessity, which insurers rely on to approve or deny requests. For instance, “Has the patient tried alternative treatments?” might be a required question for approving a more advanced procedure.
Virtual medical assistants can play a substantial role in streamlining this process. By assisting providers in gathering accurate information and formatting responses effectively, they help reduce administrative burdens while improving approval rates.
Common Challenges in Answering Clinical Questions
Even small clinics face hurdles when responding to these questions. Incomplete patient records, ambiguous insurance guidelines, and tight deadlines are common challenges. Also, providers often struggle with the sheer volume of requests, leaving room for error in documentation.
Why Accuracy is Key in Responding
Errors in clinical question responses, no matter how small, can lead to claim denials or prolonged delays. Inconsistent information, such as mismatched diagnoses or treatment plans, may raise red flags for insurers. Adopting robust Revenue Cycle Management (RCM) practices ensures that healthcare providers respond with accuracy, reducing these risks significantly.
Streamlining Prior Authorization in Atlanta
Managing prior authorization requests efficiently requires using the right tools, strategies, and expertise. For Atlanta-based providers, leveraging healthcare outsourcing and technology can simplify this process.
Leveraging Virtual Medical Assistants and Healthcare Outsourcing
Virtual medical assistants offer a practical way to manage clinical questions in a fast-paced environment. By organizing patient data and providing relevant answers promptly, they minimize errors and improve efficiency. Additionally, healthcare outsourcing supports clinics by handling complex tasks like data entry, claims processing, and eligibility verification. You can read more about this in Outsourcing in Medical Healthcare – Staffingly, Inc..
Pairing virtual assistants with healthcare BPO solutions streamlines the process, allowing providers to focus more on patient care.
Role of Insurance Verification and Provider Credentialing
Insurance verification identifies coverage details before authorization submissions, helping to avoid surprises later. Ensuring provider credentialing is up-to-date also prevents avoidable delays. For a detailed guide on this, check out What Are the Best Practices for Medical Insurance Verification.
Strategic pre-approval checks give providers confidence that their submissions align with insurers’ requirements, enhancing approval rates.
Automating Documentation and Approval Pipelines
Automation tools reduce the manual labor involved in prior authorization by streamlining document submission and approval tracking. This not only saves time but also elevates accuracy. When paired with effective healthcare outsourcing, automation transforms complex workflows into manageable systems.
The Impact on Revenue Cycle Management (RCM)
Effective handling of clinical questions doesn’t just improve patient outcomes; it has a ripple effect on financial health for healthcare providers.
Preventing Denials Through Efficient Prior Authorization
Accurately answering clinical questions weeds out potential reasons for denial, ensuring claims are reimbursed quickly. By streamlining responses, Atlanta providers can see measurable improvements in approval rates and decreased administrative headaches. For more insights, visit Insurance Verification and Its Impact on Revenue Cycle Management.
Improving Cash Flow and Sustainability
Timely approvals lead to quicker reimbursements, directly supporting better cash flow. By addressing clinical questions with precision and harnessing RCM tools, providers can create sustainable financial systems. To learn more about this connection, explore RCM and Healthcare Sustainability – Staffingly, Inc..
Conclusion
Handling clinical questions in prior authorization is no longer just about meeting insurer requirements—it’s about ensuring operational excellence and financial health. Atlanta providers stand to benefit greatly from integrating virtual medical assistants, automating workflows, and leveraging healthcare outsourcing options. By embracing these solutions, practitioners can focus on what truly matters: delivering exceptional patient care while maintaining a thriving revenue cycle. If you’re looking to simplify your prior authorization processes, now is the time to explore these strategies.
What Did We Learn?
Handling clinical questions in prior authorization is more than just a formality—it’s a crucial step in ensuring timely approvals, reducing claim denials, and keeping a practice financially healthy. Accuracy in responses, efficient data management, and leveraging tools like virtual medical assistants can make the process smoother for healthcare providers in Atlanta. By adopting the right strategies, including automation, outsourcing, and pre-approval checks, providers can focus more on patient care while maintaining a strong revenue cycle.
What People Are Asking?
1. What are clinical questions in prior authorization?
Clinical questions request specific details about a patient’s medical history, diagnosis, or treatment plan to justify the necessity of a requested service or procedure.
2. Why are clinical questions important in prior authorization?
These questions help insurers determine whether a treatment is medically necessary, ensuring appropriate care while preventing unnecessary costs.
3. What challenges do providers face in answering clinical questions?
Common challenges include incomplete patient records, unclear insurance requirements, and high administrative workloads, which can lead to delays or denials.
4. How can virtual medical assistants help with prior authorization?
Virtual medical assistants streamline the process by organizing patient data, ensuring accurate responses, and reducing administrative burdens.
5. How does accurate prior authorization impact revenue cycle management?
Properly handling clinical questions minimizes denials, speeds up approvals, and improves cash flow, contributing to a more sustainable financial system for healthcare providers.
Disclaimer
For informational purposes only; not applicable to specific situations.
For tailored support and professional services,
please contact Staffingly, Inc. at (800) 489-5877
Email : support@staffingly.com.
About This Blog : This Blog is brought to you by Staffingly, Inc., a trusted name in healthcare outsourcing. The team of skilled healthcare specialists and content creators is dedicated to improving the quality and efficiency of healthcare services. The team passionate about sharing knowledge through insightful articles, blogs, and other educational resources.
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!
 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



