On-Demand Outsourcing BPO Services for Healthcare Providers With 24/7 Coverage!
Save up to 70% on staffing costs!
Browse Specialty Staffing Services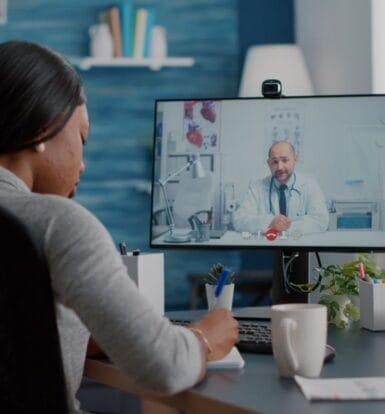
How Virtual Medical Assistants Revolutionize Telemedicine Service?
Telemedicine has become a cornerstone of modern healthcare, offering patients convenience, accessibility, and timely care. Yet, behind every successful telemedicine practice lies a team that ensures smooth operations. Virtual Medical Assistants (VMAs) have emerged as key players in supporting telemedicine services. These skilled professionals work remotely to handle a variety of tasks, helping providers focus on delivering patient care. In this article, we’ll explore the role of VMAs in telemedicine, the tasks they manage, and the benefits they bring to

How Outsourcing Solves Coding Error Challenges?
Medical coding errors might seem like small missteps, but they can create ripple effects that disrupt workflows, delay reimbursements, and even risk compliance penalties. For healthcare providers, understanding and addressing these errors is essential to maintain financial stability and deliver quality care. In this article, we’ll explore the most frequent coding mistakes, their impact on your practice, and actionable steps to avoid them. Plus, discover how outsourcing with Staffingly, Inc. can help you eliminate these errors entirely. Key Takeaways Coding

What Are the Solutions to Insurance Challenges in LTC Pharmacy Billing?
Insurance billing in long-term care (LTC) pharmacies is a complex process, often hindered by claim rejections, regulatory challenges, and time-intensive procedures. Addressing these issues requires a combination of modern technology, expert intervention, and streamlined processes. By adopting effective solutions, pharmacies can overcome these hurdles, improve efficiency, and ensure timely reimbursements. Key Takeaways: Common insurance billing challenges in LTC pharmacies include rejections, compliance complexities, and resource-heavy manual processes. Outsourcing and automation offer robust solutions to streamline billing operations. Staffingly, Inc. provides

Why Is Accurate Coding Crucial for Prior Authorizations?
In today’s complex healthcare system, prior authorizations are a necessary step for many treatments and services. However, without accurate coding, the process can become an administrative bottleneck. Incorrect or incomplete codes can delay approvals, interrupt patient care, and cause unnecessary frustrations for healthcare providers and patients alike. This article dives into why precise coding is critical for prior authorizations, how it streamlines approvals, and why outsourcing to experts like Staffingly, Inc. can enhance efficiency and compliance. Key Takeaways Accurate coding

Why LTC Pharmacies Should Outsource Their Billing Operations Today?
Running a Long-Term Care (LTC) pharmacy involves navigating a complex billing process. From ensuring accurate claims to managing denials, the billing landscape requires precision, time, and a skilled workforce. However, the increasing cost of managing in-house billing teams, coupled with ever-changing regulatory requirements, poses a significant challenge to LTC pharmacies. Outsourcing these services can be a game-changer, providing financial relief, operational efficiency, and improved accuracy. Let’s dive deeper into how outsourcing LTC pharmacy billing can help cut costs while optimizing

How Do You Handle Xtandi Prior Authorization?
How Do You Handle Xtandi Prior Authorization? 🩺📋𝗛𝗼𝘄 𝗗𝗼 𝗬𝗼𝘂 𝗛𝗮𝗻𝗱𝗹𝗲 𝗫𝘁𝗮𝗻𝗱𝗶 𝗣𝗿𝗶𝗼𝗿 𝗔𝘂𝘁𝗵𝗼𝗿𝗶𝘇𝗮𝘁𝗶𝗼𝗻? 🩺📋 Read Full Article : https://staffingly.com/xtandi-prior-authorization-key-steps-you-should-know/ Navigating the prior authorization process for Xtandi (enzalutamide) can feel overwhelming, but it doesn’t have to be. This comprehensive guide walks healthcare providers through every step, ensuring you’re equipped to secure timely approval for this life-changing prostate cancer treatment. 💡 What You’ll Learn in This Video:• How to understand insurance policies and identify key requirements for Xtandi.• Tips for

How to Overcome Insurance Challenges for Genotropin Approvals?
Dealing with insurance prior authorization (PA) for medications like Genotropin can feel overwhelming, especially when facing varying requirements from different insurance companies. But as someone who’s navigated this process, let me walk you through it step by step. Together, we’ll make the complicated feel simple and manageable. Genotropin, a synthetic growth hormone used to treat growth-related disorders, is life-changing for many patients—but its high cost often triggers strict insurance guidelines. Let’s explore why prior authorization is essential and break down

How to Simplify Norditropin Prior Authorization for Patients?
The prior authorization (PA) process for Norditropin doesn’t have to feel like climbing a mountain. As a healthcare provider, you are the guide, ensuring your patients get the growth hormone therapy they need for conditions like Growth Hormone Deficiency (GHD) or Turner syndrome. With a clear understanding of the process, you can make this journey smooth and manageable. Let’s break it all down, step by step, into something simple, conversational, and effective. Understanding Insurance Company Policies Different insurers have different
 Book a Demo to Build Your Team Today!
Book a Demo to Build Your Team Today!


 Read Case Studies
Read Case Studies 



 Virtual Medical Assistants
Virtual Medical Assistants



